Urothelial Carcinoma: Causes, Symptoms, and Treatment
What Is Urothelial Carcinoma?
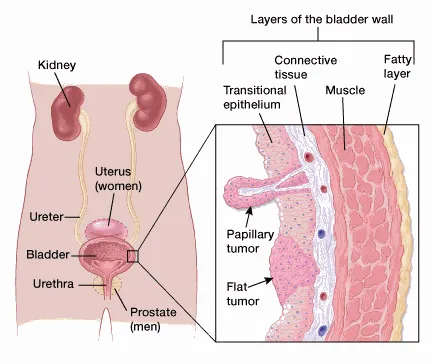
This cancer originates from urothelial cells – the epithelial lining of the urinary tract, including the bladder, renal pelvis, and ureter. Because this lining is exposed to urine and potentially harmful substances filtered by the kidneys, it is particularly prone to developing malignant changes.
How Urothelial Carcinoma Affects the Urinary System
In the Bladder
Abnormal cells first develop in the inner mucosal layer. Over time, they can invade the muscle wall and surrounding fat. Without treatment, tumor cells may spread to regional lymph nodes or distant organs such as the bones, lungs, or liver.
- High-grade bladder tumors are aggressive, more likely to invade muscle, metastasize, and threaten life.
- Low-grade bladder tumors tend to recur but rarely invade deeper layers or spread elsewhere.
In the Renal Pelvis and Ureter
Malignant urothelial cells can also form tumors in the upper urinary tract—within the renal pelvis or ureters. These tumors can obstruct urine flow and impair kidney function, sometimes leading to renal failure. Like bladder tumors, they may metastasize to other organs if untreated.
Common Signs and Symptoms
Urothelial carcinoma often causes no obvious symptoms in its earliest stages. As the disease progresses, patients may experience:
- Hematuria (blood in urine): The most frequent sign. It can be gross (visible to the naked eye) or microscopic (detected only by urinalysis).
- Painful or burning urination: Dysuria may mimic urinary tract infection.
- Increased urinary frequency or urgency: Especially nocturia.
- Flank or back pain: Persistent dull pain, particularly on one side, may indicate upper tract involvement.
- Unexplained fatigue or weight loss: Systemic manifestations of cancer.
- Low-grade persistent fever.
- Palpable abdominal or flank mass: In advanced disease, a mass near the kidney region may be felt.

Possible Complications
If not promptly diagnosed and managed, urothelial carcinoma can lead to serious complications:
- Local invasion and metastasis: Tumors may infiltrate surrounding tissues, lymph nodes, and distant organs such as lungs, liver, bones, or even the brain.
- Urinary tract obstruction: Masses in the renal pelvis, ureter, or bladder can cause hydronephrosis, reduced renal function, or even kidney failure.
- Recurrent infections: Blocked urine flow creates a favorable environment for bacteria, increasing the risk of chronic urinary tract infections or, rarely, sepsis.
- Treatment-related effects: Surgical removal of an affected kidney may reduce renal reserve. Chemotherapy and radiotherapy can cause fatigue, immunosuppression, or damage to healthy tissue.
When to Seek Medical Attention
You should consult a healthcare provider promptly if you experience:
- Any episode of blood in urine – even a single painless occurrence.
- Persistent burning or pain with urination or ongoing nocturia.
- Unexplained flank or abdominal pain.
- Unexplained weight loss or prolonged fatigue.
- Recurrent urinary tract infections that do not respond to treatment.
- A new lump or mass felt in the abdomen or flank.
Causes and Risk Factors of Urothelial Carcinoma
What Causes Urothelial Carcinoma?
The exact cause of urothelial carcinoma is not fully understood. However, research has identified several environmental and genetic factors that increase susceptibility. The urothelium is constantly exposed to substances filtered by the kidneys, making it vulnerable to carcinogens and chronic irritation.
Who Is at Higher Risk?
Individuals more likely to develop urothelial carcinoma include:
- Tobacco users: Cigarette smoking is the strongest known risk factor. Carcinogenic chemicals from tobacco are filtered by the kidneys and concentrated in urine, directly damaging the lining of the urinary tract.
- Occupational exposure to toxic chemicals: Workers in dye, rubber, leather, paint, textile, petrochemical, or steel industries—and even some hairdressers regularly exposed to styling chemicals—have an elevated risk due to contact with aromatic amines and other carcinogens.
- History of chemotherapy or pelvic radiotherapy: Drugs such as cyclophosphamide or radiation treatment to the pelvic area (e.g., for prostate cancer) can increase the likelihood of developing bladder or upper tract tumors years later.
- Chronic bladder inflammation: Long-term indwelling catheters or recurrent urinary tract infections may chronically irritate the urothelium, promoting malignant transformation.
- Arsenic in drinking water: Prolonged exposure to arsenic, a potent carcinogen, is associated with urothelial cancers in some regions.
- Inherited syndromes and genetic mutations: People with Lynch syndrome or a strong family history of urinary tract cancers face a higher lifetime risk.

Diagnostic Evaluation of Urothelial Carcinoma
Because early-stage urothelial carcinoma can be asymptomatic, accurate diagnosis relies on a combination of medical history, physical examination, and targeted tests. Common investigations include:
- Urinalysis: Assesses urine for color, protein, glucose, blood, and signs of infection.
- Urine cytology: Examines urine under a microscope to detect cancer cells shed from the bladder, ureter, or renal pelvis.
- Intravenous urography (IVU) with contrast X-ray: A contrast dye is injected into a vein to outline the urinary tract on X-ray and reveal blockages or masses.
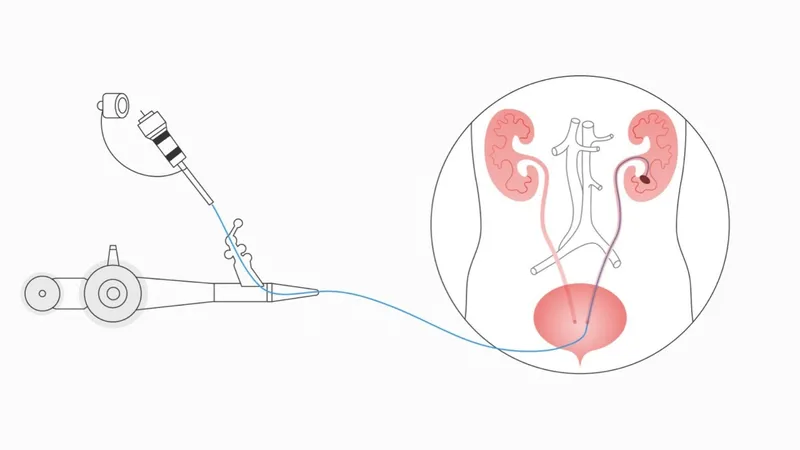
- Ureteroscopy: A thin, lighted scope is passed through the bladder into the ureter and renal pelvis to directly visualize lesions and obtain biopsies.
- Computed tomography (CT) scan: Provides detailed cross-sectional images of the kidneys, bladder, and surrounding structures to detect tumors and metastases.
- Ultrasound: Uses sound waves to create images of the kidneys, bladder, and ureters, helping identify masses or obstruction.
- Magnetic resonance imaging (MRI): Generates high-resolution images using magnetic fields and radio waves, particularly useful for evaluating local tumor invasion.
Treatment of Urothelial Carcinoma
Management of urothelial carcinoma depends on the tumor’s location, stage, grade, the patient’s overall health, and personal preferences. A multidisciplinary approach combining surgery, systemic therapy, and local treatments is often used.
Management of Bladder Urothelial Carcinoma
Surgical Options
- Transurethral Resection (TURBT): For non–muscle-invasive tumors, the lesion is removed or cauterized through a cystoscope passed via the urethra.
- Partial or Radical Cystectomy: In muscle-invasive disease, part or all of the bladder may need to be surgically removed. Pelvic lymph node dissection is often performed simultaneously. Urinary diversion (e.g., ileal conduit or neobladder) may be created after total cystectomy.
Intravesical Therapy
- Immunotherapy with Bacillus Calmette–Guérin (BCG): Delivered directly into the bladder to stimulate the immune system and reduce recurrence.
- Intravesical Chemotherapy: Agents such as mitomycin C or gemcitabine can be instilled to destroy residual tumor cells after surgery.
Systemic Chemotherapy
- Used before surgery (neoadjuvant) to shrink tumors or after surgery (adjuvant) to kill remaining cancer cells.
- Common regimens include cisplatin-based combinations.
Radiation Therapy
- High-energy beams destroy cancer cells. May be used for patients who are not surgical candidates or as part of bladder-sparing protocols.
Targeted and Immunotherapy Agents
- Newer drugs, such as immune checkpoint inhibitors (e.g., pembrolizumab, atezolizumab), target specific pathways in tumor growth or enhance immune response, particularly for advanced or metastatic disease.
Management of Upper Tract (Kidney, Renal Pelvis, Ureter) Urothelial Carcinoma
Surgery
- Nephroureterectomy: Standard treatment for high-grade tumors involves removal of the kidney, renal pelvis, ureter, and a cuff of bladder.
- Segmental Resection or Endoscopic Ablation: For select low-risk lesions, conservative approaches may preserve renal function.
Systemic Therapy
- Platinum-based chemotherapy or immunotherapy may be indicated in advanced or recurrent disease.
Ablative Techniques
- Cryoablation: Freezing the tumor with extreme cold to destroy cancer cells.
- Radiofrequency Ablation (RFA): Using high-frequency energy to heat and destroy malignant tissue, mainly in small renal masses.
Intravesical and Local Therapies
For non–muscle-invasive disease, intravesical administration of chemotherapy or immunotherapy directly into the bladder remains a cornerstone. This approach significantly lowers recurrence rates when the cancer is confined to the mucosal layer.

Lifestyle and Prevention Strategies for Urothelial Carcinoma
Although no single measure can completely prevent urothelial carcinoma, a healthy lifestyle can support treatment outcomes, improve quality of life, and lower the risk of recurrence.
Healthy Habits During and After Treatment
- Adhere to your treatment plan: Attend follow-up visits as scheduled, take prescribed medications, and complete recommended therapies exactly as directed by your healthcare team.
- Maintain good personal and urinary hygiene: Keep the genital area clean to reduce the risk of infection. Unless otherwise instructed by your physician, drink 2–2.5 liters of water daily to help flush the urinary tract.
- Manage stress: Practice relaxation techniques such as meditation, yoga, or deep breathing. Gentle hobbies like reading or painting can also improve emotional well-being.
- Engage in light physical activity: Walking, swimming, or yoga may boost energy, strengthen immunity, and enhance mood.
- Monitor symptoms: Record any unusual changes such as blood in urine, new pain, persistent fever, or unusual fatigue, and inform your healthcare provider promptly.
- Quit smoking: Tobacco is the strongest modifiable risk factor for recurrence and new tumors.
- Limit exposure to hazardous chemicals: Avoid working with or protect yourself from paints, dyes, rubber, petroleum products, and other industrial toxins whenever possible.

Nutrition Recommendations
Foods to Include:
- High-quality protein: Fish, poultry, eggs, beans, nuts, and dairy help maintain muscle mass and tissue repair.
- Colorful vegetables and fruits: Broccoli, spinach, carrots, apples, berries, and citrus fruits provide antioxidants and vitamins that support the immune system.
- Whole grains: Oats, brown rice, and whole-grain bread supply fiber and steady energy.
- Healthy fats: Olive oil, avocados, salmon, and mackerel support cardiovascular and overall health.
- Hydrating foods: Watermelon, cucumber, and vegetable soups can contribute to fluid intake and urinary tract cleansing.
Foods to Limit:
- Processed and fast foods: High in salt, sugar, and preservatives.
- Red and fried meats: Reduce intake of fatty cuts, sausages, and fried foods to lower inflammation and potential cancer risk.
- Alcohol and stimulants: Limit or avoid alcohol, beer, and coffee unless approved by your doctor.
Reducing Your Risk of Urothelial Carcinoma
While complete prevention is not possible, you can significantly lower risk by:
- Quitting tobacco use: The single most important step to reduce both primary risk and recurrence.
- Avoiding toxic chemical exposure: Use protective equipment or change work environments where dyes, rubber, paints, or industrial chemicals are handled.
- Staying well hydrated: Adequate fluid intake dilutes and flushes carcinogens from the urinary tract.
- Eating a plant-rich, antioxidant-dense diet: Emphasize fresh produce and minimize processed foods and saturated fats.
- Managing chronic urinary conditions: Promptly treat recurrent bladder infections, kidney stones, or other urinary tract disorders to minimize long-term irritation and potential malignant changes.

