Stage 1 Colon Cancer: Symptoms, Causes, Diagnosis and Treatment
Overview of Stage 1 Colon Cancer
The colon is part of the gastrointestinal tract, which also includes the esophagus, stomach, small intestine, and large intestine. The colon constitutes the main part of the large intestine, about 5 feet (1.5 m) long. Together with the rectum and anal canal, it forms the large bowel. The digestive system processes nutrients (vitamins, minerals, carbohydrates, fats, proteins, and water) from food and eliminates waste.
According to the American Cancer Society, approximately 1 in 23 men and 1 in 25 women will develop colorectal cancer in their lifetime.
Stage 1 colon cancer means the tumor has penetrated the inner lining or mucosa of the colon and may extend into the muscular layer but has not spread to nearby lymph nodes or distant organs. Most colon cancers are diagnosed in the early stages (Stages 1–3), which provides a strong opportunity for cure.
Symptoms of Stage 1 Colon Cancer
Signs and Symptoms
In the early stages, such as Stage 1 colon cancer, you may have no symptoms at all. When present (usually in Stages 0–2), symptoms may include:
- Constipation
- Diarrhea
- Change in stool color
- Change in stool shape, e.g., pencil-thin stools
- Blood in stool
- Abdominal pain
- Cramping
These symptoms are nonspecific and may result from many other conditions. It is important to see a doctor for accurate diagnosis.
Potential Complications
If left undiagnosed or untreated, Stage 1 colon cancer can progress to more advanced stages.
When to See a Doctor
If you experience the above symptoms lasting 1–2 weeks, consult your physician. Symptoms such as constipation, diarrhea, blood in stool, or abdominal pain can also signal less serious conditions. However, only proper evaluation can determine whether colorectal cancer screening is needed.
Causes of Stage 1 Colon Cancer
The causes of Stage 1 colon cancer mirror those of colon cancer overall:
Sporadic cases (≈70%): usually related to environmental and lifestyle factors, occurring mostly in individuals over age 50.
Familial clustering (≈20%).
Inherited syndromes (≈10%): occur at younger ages (under 50) with much higher risk.
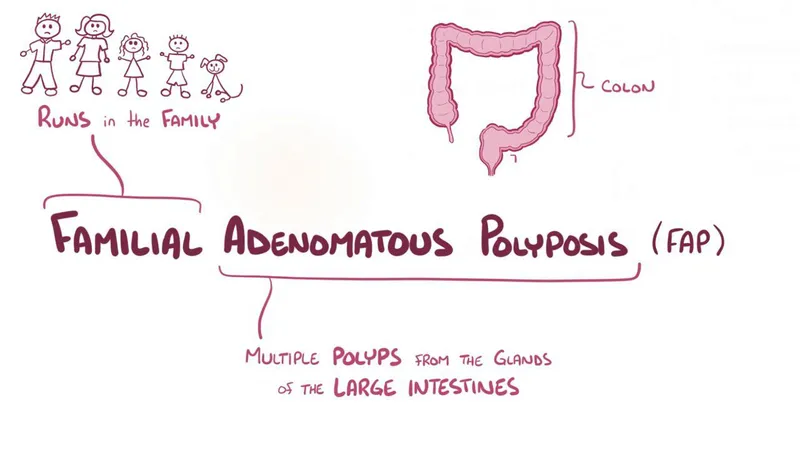
The most common inherited syndromes linked to colon cancer are familial adenomatous polyposis (FAP) and Lynch syndrome (hereditary non-polyposis colorectal cancer, HNPCC). Together they account for about 5% of all colorectal cancers.
Risk Factors for Stage 1 Colon Cancer
Who Is at Risk?
Anyone can develop Stage 1 colon cancer. Risk is higher with family history, genetic syndromes, or certain lifestyle and environmental exposures.
Epidemiological data show higher rates of colorectal cancer in developed countries. Lower socioeconomic status correlates with increased risk due to high-risk behaviors and limited access to healthcare. In White Americans, men have higher colorectal cancer incidence than women.
Risk-Enhancing Factors
Risk factors for colon cancer also apply to Stage 1 disease:
Personal or family history of colorectal cancer or adenomatous polyps.
Inflammatory bowel disease (IBD): Ulcerative colitis carries a clear link, with estimated incidence of 0.5% per year 10–20 years after diagnosis.
Crohn’s disease: particularly involving the terminal ileum increases colon cancer risk.
Childhood cancer survivors who received abdominal radiation should begin screening 10 years later or at age 35.
Other conditions: diabetes, insulin resistance, uncontrolled acromegaly, long-term immunosuppression after kidney transplantation.

Lifestyle factors strongly associated with colon cancer include:
- Obesity
- Red or processed meat consumption
- Tobacco use
- Alcohol intake
- Androgen deprivation therapy (for prostate cancer)
- Prior cholecystectomy
Diagnosis of Stage 1 Colon Cancer
Screening and Diagnostic Tests
Diagnosing colon cancer early, such as at Stage 1, greatly increases the chance of cure. Because Stage 1 disease often causes no symptoms, it is frequently detected during routine screening.
Colonoscopy: Detects most colon cancers, with about 80% diagnosed in symptomatic individuals. About 11% are found through asymptomatic screening and 7% incidentally during emergency hospitalization.
History and physical examination: Assess personal and family history.
Barium enema or CT colonography: Initial imaging options.
Biopsy: All suspicious lesions must be biopsied and examined histopathologically to confirm diagnosis.
Treatment of Stage 1 Colon Cancer
Stage 1 colon cancer has invaded the mucosa or muscular layer but not beyond the bowel wall or to lymph nodes.
Surgery is the main treatment: Removing the tumor and surrounding tissue. Most Stage 1 patients do not need adjuvant chemotherapy after surgery.

Chemotherapy: Not indicated for Stage 1 disease.
Radiotherapy ± chemotherapy: Considered only for patients unable to undergo surgery due to frailty or small tumor location.

Treatment may be adjusted after surgery if pathology shows more advanced disease.
Lifestyle and Prevention
Healthy Habits During and After Treatment
For best outcomes, early diagnosis and treatment are crucial. The American Cancer Society reports a 91% five-year survival rate for colon cancer diagnosed before metastasis.
All patients undergoing and after completing treatment should adopt healthy lifestyle changes:
- Eat a balanced, healthy diet.
- Achieve and maintain ideal body weight.
- Establish a regular exercise routine.
- Limit alcohol and quit smoking.
Effective Prevention Strategies
Large population studies suggest protective factors against colon cancer include:
- Physical activity
- Dietary measures: fruits, vegetables, fiber, resistant starch, fish
- Supplementation: folate, folic acid, vitamin B6 (pyridoxine), calcium, vitamin D, magnesium
- Garlic
- Coffee
Certain medications also show preventive effects:
- Aspirin and non-steroidal anti-inflammatory drugs (NSAIDs)
- Menopausal hormone replacement therapy
- Statins
- Angiotensin inhibitors
- Bisphosphonates

Notably, a randomized controlled trial demonstrated that 600 mg aspirin in Lynch syndrome patients significantly reduced colorectal adenoma and cancer incidence after 55.7 months (p=0.05).
