Comprehensive Guide to Rocuronium: Uses, Dosage, Side Effects, and More
1. What is Rocuronium?
2. Overview of Rocuronium
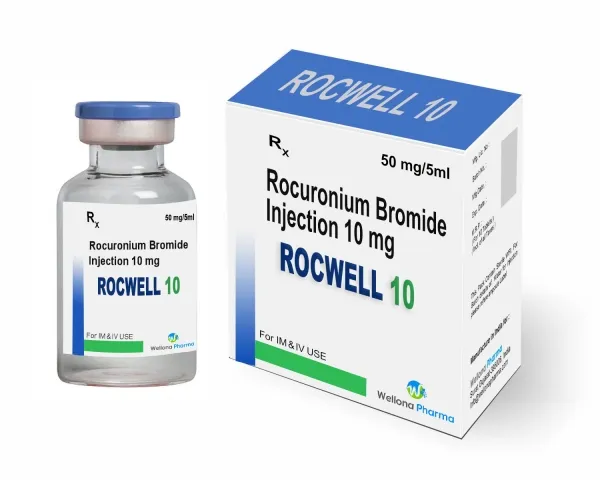
Generic Name
Rocuronium
Brand Name
Zemuron, generics
Drug Group
Non-depolarizing neuromuscular blocker
Commonly Used For
This medication is used to:
- Facilitate endotracheal intubation.
- Provide skeletal muscle relaxation during surgery.
- Assist with mechanical ventilation in critical care.
Key Characteristics
- Form: Intravenous solution (10 mg/mL) (detailed in Dosage section).
- Mechanism: Competes with acetylcholine at nicotinic receptors, inducing paralysis.
- Approval: FDA-approved (1994 for Zemuron) and EMA-approved for anesthesia and critical care.
3. Indications and Uses of Rocuronium
Rocuronium is indicated for various clinical scenarios requiring muscle relaxation, leveraging its rapid onset and intermediate duration:
- Endotracheal Intubation: Facilitates rapid sequence intubation in emergency settings (e.g., trauma, airway obstruction), providing optimal conditions within 60 seconds, per anesthesia guidelines.
- Surgical Muscle Relaxation: Maintains skeletal muscle relaxation during general anesthesia for procedures like abdominal surgery, orthopedic interventions, or neurosurgery, enhancing surgical precision.
- Mechanical Ventilation: Supports controlled ventilation in intensive care units (ICUs) for patients with acute respiratory distress syndrome (ARDS) or status asthmaticus, improving oxygenation, supported by critical care protocols.
- Elective Surgery: Used in elective surgeries (e.g., appendectomy, hernia repair) to optimize operating conditions, reducing patient movement, with data from perioperative studies.
- Neuromuscular Disease Management: Employed off-label to manage spasticity or rigidity in conditions like tetanus or severe cerebral palsy, under neurologist supervision, with emerging evidence.
- Pediatric Anesthesia: Administered off-label in children (including neonates) for intubation or surgery, adjusting doses for safety, supported by pediatric anesthesia research.
- Cardiac Surgery: Used off-label during cardiopulmonary bypass to prevent patient movement, improving surgical outcomes, with cardiology and thoracic surgery data.
- Status Epilepticus: Investigated off-label as an adjunct to control muscle activity in refractory status epilepticus, enhancing EEG monitoring, noted in neurology studies.
- Burn Injury Management: Explored off-label in burn patients requiring prolonged ventilation, managing hypermetabolic response, with burn care evidence.
Note: This drug requires monitoring with a peripheral nerve stimulator; consult a healthcare provider for administration and reversal strategies.
4. Dosage of Rocuronium
Important Note: The dosage of this neuromuscular blocker must be prescribed by a healthcare provider. Dosing varies by indication, patient weight, and clinical context, with adjustments based on neuromuscular monitoring.
Dosage for Adults
- Endotracheal Intubation:
- Initial: 0.6 mg/kg IV (standard dose) or 1.0–1.2 mg/kg IV (rapid sequence), administered over 5–15 seconds.
- Maintenance of Neuromuscular Block:
- 0.1–0.2 mg/kg IV every 15–30 minutes, titrated to response.
- Long-Term ICU Use:
- 0.1–0.2 mg/kg IV every 1–2 hours, adjusted with train-of-four monitoring.
Dosage for Children
- Neonates to 3 months:
- 0.45–0.6 mg/kg IV for intubation, under pediatric anesthesiologist supervision.
- 3 months to 12 years:
- 0.6–1.0 mg/kg IV for intubation; 0.075–0.125 mg/kg for maintenance.
- 12–17 years:
- Adult dosing (0.6–1.2 mg/kg IV), adjusted for weight.
Dosage for Pregnant Women
- Pregnancy Category C: Use only if benefits outweigh risks (e.g., emergency surgery). Consult an obstetrician, with fetal monitoring.
Dosage Adjustments
- Renal Impairment: No adjustment needed; monitor in severe cases (CrCl <30 mL/min).
- Hepatic Impairment: No adjustment needed; monitor for prolonged effects in severe cases (Child-Pugh C).
- Elderly: Start with 0.6 mg/kg IV; increase cautiously to 1.0 mg/kg if needed.
- Obesity: Use ideal body weight for dosing; adjust based on clinical response.
Additional Considerations
- Administer this active ingredient via IV bolus or infusion by an anesthesiologist.
- Use a peripheral nerve stimulator to assess depth of block and guide reversal.
5. How to Use Rocuronium
- Administration:
- Inject IV bolus over 5–15 seconds or infuse via a calibrated pump; avoid intramuscular use.
- Administer in a controlled setting with airway management equipment and reversal agents (e.g., neostigmine) available.
- Timing: Use as a single dose for intubation or as repeated doses for maintenance, guided by neuromuscular monitoring.
- Monitoring: Continuously assess with a peripheral nerve stimulator (e.g., train-of-four) to evaluate block depth and recovery.
- Additional Tips:
- Store at 20–25°C (68–77°F); protect from light and freezing.
- Keep out of reach of children due to toxicity risk.
- Report prolonged weakness, difficulty breathing, or signs of allergic reaction immediately.
6. Contraindications for Rocuronium
This drug is contraindicated in:
- Hypersensitivity: Patients with a known allergy to Rocuronium or other aminosteroid neuromuscular blockers.
- Myasthenia Gravis: Contraindicated due to exaggerated paralysis risk.
- Severe Electrolyte Imbalance: Avoid in uncontrolled hyperkalemia or hypocalcemia.
7. Warnings & Precautions for Rocuronium
General Warnings
- Residual Paralysis: Risk of prolonged neuromuscular block; ensure complete reversal before extubation.
- Anaphylaxis: Rare but severe risk; have emergency drugs (e.g., epinephrine) ready.
- Hyperkalemia: Risk in burn patients or those with denervation; monitor potassium levels.
- Malignant Hyperthermia: Potential trigger; monitor temperature and muscle rigidity.
- Bradycardia: Risk with rapid administration; premedicate with anticholinergics if needed.
Additional Warnings
- Hepatic/Renal Dysfunction: Prolonged effects in severe cases; adjust monitoring.
- Pulmonary Complications: Risk of aspiration or atelectasis; ensure airway protection.
- Neurological Effects: Rare seizures with overdose; monitor EEG if suspected.
- Hypotension: Risk with rapid IV push; administer slowly.
- Hypersensitivity Reactions: Rare anaphylaxis; discontinue if swelling occurs.
Use in Specific Populations
- Pregnancy: Category C; use only if essential with fetal monitoring.
- Breastfeeding: Excreted in breast milk; monitor infant for effects.
- Elderly: Higher risk of prolonged block; start with lower doses.
- Children: Limited to neonates+; supervise closely.
- Renal/Hepatic Impairment: Monitor closely; no dose adjustment typically needed.
Additional Precautions
- Inform your doctor about neuromuscular diseases, electrolyte imbalances, or medication history before starting this medication.
- Ensure availability of reversal agents (e.g., sugammadex) and ventilatory support.
8. Overdose and Management of Rocuronium
Overdose Symptoms
Overdose may cause:
- Prolonged paralysis, respiratory depression, or apnea.
- Severe cases: Cardiovascular collapse or hyperkalemia.
- Weakness, dizziness, or difficulty swallowing as early signs.
- Cardiac arrest with extremely high doses.
Immediate Actions
- Contact the Medical Team: Seek immediate medical help.
- Supportive Care: Provide mechanical ventilation, administer reversal agents (e.g., sugammadex 16 mg/kg IV or neostigmine 0.07 mg/kg with glycopyrrolate), and monitor vital signs.
- Specific Treatment: Correct electrolytes and manage airway; no specific antidote beyond reversal.
- Monitor: Check neuromuscular function, oxygen saturation, and heart rate for 24–48 hours.
Additional Notes
- Overdose risk is high in unmonitored settings; store securely.
- Report persistent symptoms (e.g., prolonged weakness, irregular heartbeat) promptly.
9. Side Effects of Rocuronium
Common Side Effects
- Hypotension (5–15%, manageable with fluids)
- Nausea (3–10%, reduced with antiemetics)
- Muscle Weakness (2–8%, resolves with reversal)
- Bradycardia (2–7%, mitigated with anticholinergics)
- Injection Site Pain (1–5%, transient)
These effects may subside with proper management.
Serious Side Effects
Seek immediate medical attention for:
- Respiratory: Apnea, respiratory failure, or prolonged paralysis.
- Cardiovascular: Severe bradycardia, hypotension, or cardiac arrest.
- Neurological: Seizures or prolonged weakness.
- Allergic: Anaphylaxis, bronchospasm, or rash.
- Metabolic: Hyperkalemia or acidosis.
Additional Notes
- Regular monitoring with a peripheral nerve stimulator and vital signs is advised.
- Report any unusual symptoms (e.g., difficulty breathing, chest pain) immediately to a healthcare provider.
10. Drug Interactions with Rocuronium
This active ingredient may interact with:
- Anesthetics: Enhances block (e.g., volatile agents); adjust dose.
- Antibiotics: Prolongs effects (e.g., aminoglycosides); monitor closely.
- Magnesium Sulfate: Increases paralysis risk; reduce dose.
- Calcium Channel Blockers: Potentiates hypotension; monitor BP.
- Corticosteroids: May alter duration; adjust based on response.
Action: Provide your healthcare provider with a complete list of medications.
11. Patient Education or Lifestyle
- Medication Adherence: Take this neuromuscular blocker as prescribed by an anesthesiologist, typically in a controlled setting.
- Monitoring: Report prolonged weakness, breathing difficulties, or allergic signs immediately.
- Lifestyle: Avoid alcohol or sedatives post-procedure; follow recovery instructions.
- Diet: N/A for administration; resume normal diet post-reversal with guidance.
- Emergency Awareness: Know signs of respiratory distress or cardiac issues; seek care if present.
- Follow-Up: Schedule post-operative or ICU check-ups to assess recovery and neuromuscular function.
12. Pharmacokinetics of Rocuronium
- Absorption: Not orally bioavailable; administered IV (peak effect in 1–2 minutes).
- Distribution: Volume of distribution ~0.2–0.3 L/kg; 30% protein-bound.
- Metabolism: Minimal hepatic metabolism; excreted largely unchanged.
- Excretion: Primarily biliary (50–60%) and renal (30–40%); half-life 1.4–2.4 hours.
- Half-Life: 1.4–2.4 hours, with duration influenced by liver and kidney function.
13. Pharmacodynamics of Rocuronium
This drug exerts its effects by:
- Competitively binding to nicotinic acetylcholine receptors at the neuromuscular junction.
- Inducing dose-dependent skeletal muscle relaxation, with rapid onset (60–90 seconds).
- Reversible with cholinesterase inhibitors or sugammadex, depending on depth of block.
- Exhibiting variable duration based on patient factors (e.g., hepatic clearance).
14. Storage of Rocuronium
- Temperature: Store at 20–25°C (68–77°F); excursions permitted to 15–30°C (59–86°F).
- Protection: Keep in original container, away from light and freezing.
- Safety: Store in a locked container out of reach of children due to toxicity risk.
- Disposal: Dispose of unused vials per hazardous drug regulations or consult a pharmacist.
15. Frequently Asked Questions (FAQs) About Rocuronium
Q: What does Rocuronium treat?
A: This medication facilitates intubation and muscle relaxation.
Q: Can this active ingredient cause weakness?
A: Yes, muscle weakness may occur; it resolves with reversal.
Q: Is Rocuronium safe for children?
A: Yes, for neonates+ with a doctor’s guidance.
Q: How is this drug taken?
A: Via IV injection, as directed by an anesthesiologist.
Q: How long is Rocuronium effect?
A: Typically 20–40 minutes, reversible with medication.
Q: Can I use Rocuronium if pregnant?
A: Yes, with caution; consult a doctor.
16. Regulatory Information for Rocuronium
This medication is approved by:
- U.S. Food and Drug Administration (FDA): Approved in 1994 (Zemuron) for anesthesia and ICU use.
- European Medicines Agency (EMA): Approved for neuromuscular blockade.
- Other Agencies: Approved globally for anesthesia; consult local guidelines.
17. References
- U.S. Food and Drug Administration (FDA). (2023). Zemuron (Rocuronium) Prescribing Information.
- Official FDA documentation detailing the drug’s approved uses, dosage, and safety.
- European Medicines Agency (EMA). (2023). Rocuronium Summary of Product Characteristics.
- EMA’s comprehensive information on the medication’s indications and precautions in Europe.
- National Institutes of Health (NIH). (2023). Rocuronium: MedlinePlus Drug Information.
- NIH resource providing detailed information on the drug’s uses, side effects, and precautions.
- World Health Organization (WHO). (2023). WHO Model List of Essential Medicines: Rocuronium.
- WHO’s inclusion of Rocuronium for anesthesia.
- Anesthesiology. (2022). Rocuronium in Rapid Sequence Intubation.
- Peer-reviewed article on Rocuronium efficacy (note: access may require a subscription).
