Comprehensive Guide to Ranibizumab: Uses, Dosage, Side Effects, and More
What is Ranibizumab?
Overview of Ranibizumab
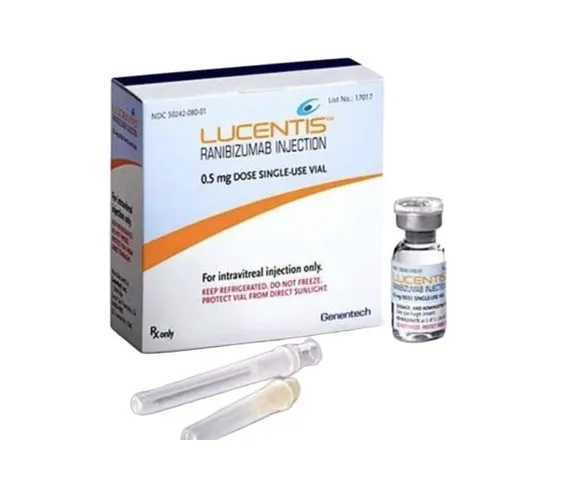
Generic Name: Ranibizumab
Brand Name: Lucentis, generics
Drug Group: Anti-VEGF agent (ophthalmic)
Commonly Used For
- Treat neovascular (wet) age-related macular degeneration (AMD).
- Manage diabetic macular edema (DME).
- Address retinal vein occlusion (RVO).
Key Characteristics
Form: Solution for intravitreal injection (0.5 mg/0.05 mL, 0.3 mg/0.05 mL) (detailed in Dosage section).
Mechanism: Binds VEGF-A, inhibiting angiogenesis and vascular permeability in the retina.
Approval: FDA-approved (2006 for Lucentis) and EMA-approved for retinal conditions.
Indications and Uses of Ranibizumab
Ranibizumab is indicated for a range of ocular conditions, leveraging its anti-angiogenic properties to stabilize or improve vision:
Neovascular (Wet) Age-Related Macular Degeneration (AMD): Treats wet AMD by inhibiting choroidal neovascularization (CNV), preserving central vision, supported by landmark trials like ANCHOR and MARINA.
Diabetic Macular Edema (DME): Manages DME in diabetic retinopathy, reducing macular thickness and improving visual acuity, per diabetic eye disease studies.
Macular Edema Following Retinal Vein Occlusion (RVO): Treats macular edema due to branch or central RVO, enhancing retinal perfusion and vision, supported by BRAVO and CRUISE trials.
Myopic Choroidal Neovascularization (mCNV): Addresses mCNV in high myopia, stabilizing vision, with evidence from RADIANCE trial data.
Diabetic Retinopathy (DR) without DME: Used off-label to slow DR progression in non-proliferative stages, improving retinal health, supported by emerging ophthalmologic research.
Retinal Angiomatous Proliferation (RAP): Investigated off-label for RAP, a subtype of wet AMD, reducing lesion growth, with data from retinal specialists.
Ocular Histoplasmosis Syndrome: Employed off-label to manage CNV secondary to histoplasmosis, preserving vision, with case studies in infectious eye disease.
Retinopathy of Prematurity (ROP): Explored off-label in severe ROP cases to reduce neovascularization, with cautious use under pediatric ophthalmology supervision.
Uveitic Macular Edema: Used off-label to treat macular edema in uveitis, improving outcomes, supported by inflammatory eye disease research.
Polypoidal Choroidal Vasculopathy (PCV): Investigated off-label for PCV, a variant of CNV, enhancing visual stability, with growing evidence from Asian and European cohorts.
Dosage of Ranibizumab
Dosage for Adults
Neovascular AMD: 0.5 mg (0.05 mL) via intravitreal injection monthly, with a loading phase of 3 monthly doses, followed by as-needed (PRN) or treat-and-extend regimens.
Diabetic Macular Edema (DME): 0.3 mg (0.05 mL) via intravitreal injection monthly, with a loading phase of 5 monthly doses, adjusted based on visual acuity and OCT findings.
Macular Edema Following RVO: 0.5 mg (0.05 mL) via intravitreal injection monthly, up to 6 months, with reassessment.
Myopic Choroidal Neovascularization (mCNV): 0.5 mg (0.05 mL) via intravitreal injection monthly until stable, then PRN.
Dosage for Children
Retinopathy of Prematurity (ROP, off-label): 0.2–0.3 mg (0.02–0.03 mL) via intravitreal injection, adjusted by weight and gestational age, under pediatric ophthalmologist supervision.
Not routinely recommended for infants.
Dosage for Pregnant Women
Pregnancy Category C: Limited data; use only if benefits outweigh risks (e.g., severe vision loss). Consult an obstetrician, with fetal monitoring.
Dosage Adjustments
Renal Impairment: No adjustment needed; monitor in severe cases (CrCl <30 mL/min).
Hepatic Impairment: No specific adjustment; use caution in severe cases.
Elderly: No adjustment needed; monitor for systemic absorption risks.
Concomitant Ocular Conditions: Adjust frequency if combined with other intravitreal therapies (e.g., corticosteroids).
Additional Considerations
- Administer this active ingredient via intravitreal injection by an ophthalmologist using aseptic technique.
- Use prophylactic antibiotics post-injection to reduce infection risk.
How to Use Ranibizumab
Administration:
Performed by an ophthalmologist via intravitreal injection into the vitreous cavity using a 30-gauge needle, following local anesthesia and antiseptic preparation.
Administer in a sterile environment, with patients positioned supine.
Timing: Use monthly or as per a treat-and-extend protocol, based on disease activity and visual outcomes.
Monitoring: Watch for eye pain, redness, or vision changes post-injection; schedule follow-up visits.
Additional Tips:
- Store at 2–8°C (36–46°F); do not freeze or shake.
- Avoid rubbing the eye post-injection; use protective eyewear if needed.
- Report severe eye pain, floaters, or signs of infection (e.g., discharge) immediately.
Contraindications for Ranibizumab
Hypersensitivity: Patients with a known allergy to Ranibizumab or its components.
Ocular or Periocular Infections: Contraindicated due to infection risk (e.g., conjunctivitis, endophthalmitis).
Active Intraocular Inflammation: Avoid in cases of uveitis or scleritis.
Severe Cardiac Conditions: Contraindicated in patients with recent myocardial infarction or stroke (due to systemic VEGF inhibition).
Side Effects of Ranibizumab
Common Side Effects
- Conjunctival Hemorrhage (20–30%, resolves spontaneously)
- Eye Pain (15–25%, manageable with rest)
- Vitreous Floaters (10–20%, transient)
- Increased Intraocular Pressure (5–15%, monitored post-injection)
- Foreign Body Sensation (5–10%, decreases over time)
These effects may subside with subsequent injections.
Serious Side Effects
Seek immediate medical attention for:
- Infectious: Endophthalmitis or conjunctivitis.
- Retinal: Detachment, tears, or hemorrhage.
- Cardiovascular: Stroke, myocardial infarction, or hypertension.
- Ocular: Cataract progression or severe inflammation.
- Allergic: Rash, angioedema, or anaphylaxis.
Additional Notes
- Regular monitoring for retinal structure, IOP, and systemic effects is advised.
- Report any unusual symptoms (e.g., sudden vision loss, chest pain) immediately to a healthcare provider.
Warnings & Precautions for Ranibizumab
General Warnings
Endophthalmitis: Risk of severe eye infection; use aseptic technique.
Retinal Detachment: Rare risk post-injection; monitor for flashes or floaters.
Increased Intraocular Pressure (IOP): Temporary elevation; check IOP post-injection.
Thromboembolic Events: Risk of stroke or myocardial infarction; screen at-risk patients.
Cataract Formation: Increased risk with repeated injections; monitor lens status.
Additional Warnings
Vitreous Hemorrhage: Rare bleeding risk; assess pre-injection.
Ocular Inflammation: Risk of uveitis or iritis; treat promptly.
Systemic VEGF Inhibition: Potential impact on wound healing; inform patients.
Retinal Pigment Epithelial Tears: Risk in patients with pigment epithelium detachment; monitor closely.
Hypersensitivity Reactions: Rare anaphylaxis; discontinue if swelling occurs.
Use in Specific Populations
- Pregnancy: Category C; avoid unless critical; use contraception.
- Breastfeeding: Avoid due to potential systemic absorption; monitor infant.
- Elderly: Higher risk of systemic effects; monitor cardiovascular health.
- Children: Limited to off-label ROP use; supervise closely.
- Renal/Hepatic Impairment: No adjustment needed; monitor systemic effects.
Additional Precautions
- Inform your doctor about eye infections, heart disease, or recent surgeries before starting this medication.
- Avoid driving immediately post-injection due to temporary vision changes.
Overdose and Management of Ranibizumab
Overdose Symptoms
- Increased intraocular pressure, eye pain, or vision loss.
- Severe cases: Endophthalmitis, retinal detachment, or systemic VEGF effects.
- Redness, floaters, or discomfort as early signs.
- Systemic symptoms (e.g., hypertension) with excessive doses.
Immediate Actions
Contact the Medical Team: Seek immediate medical help.
Supportive Care: Monitor IOP, administer antibiotics if infected, and provide symptomatic relief.
Specific Treatment: No antidote; manage complications (e.g., vitrectomy for detachment).
Monitor: Check vision, IOP, and retinal status for 7–14 days.
Additional Notes
- Overdose risk is low with proper dosing; store securely.
- Report persistent symptoms (e.g., severe vision loss, eye swelling) promptly.
Drug Interactions with Ranibizumab
This active ingredient may interact with:
- Anticoagulants: Increases bleeding risk (e.g., warfarin); monitor INR.
- Antiplatelet Agents: Enhances hemorrhage risk (e.g., aspirin); use cautiously.
- Corticosteroids: Potentiates IOP elevation; adjust dosing.
- Other Anti-VEGF Agents: Risk of cumulative systemic effects; avoid overlap.
- Immunosuppressants: May alter immune response; monitor closely.
Action: Provide your healthcare provider with a complete list of medications.
Patient Education or Lifestyle
Medication Adherence: Receive this anti-VEGF agent as prescribed by an ophthalmologist, following the injection schedule.
Monitoring: Report eye pain, vision changes, or redness immediately.
Lifestyle: Avoid rubbing the eye post-injection; wear sunglasses in bright light.
Diet: No specific restrictions; maintain a balanced diet for eye health.
Emergency Awareness: Know signs of infection or retinal detachment (e.g., flashes, floaters); seek care if present.
Follow-Up: Schedule regular eye exams every 4–8 weeks during therapy to monitor retinal health and visual acuity.
Pharmacokinetics of Ranibizumab
Absorption: Minimal systemic absorption post-intravitreal injection; local effect in the vitreous.
Distribution: Volume of distribution ~4.5 mL in the vitreous; minimal plasma levels (<0.5 ng/mL).
Metabolism: Degraded by proteolysis in the eye; no significant hepatic metabolism.
Excretion: Cleared via systemic circulation with a half-life of ~9 days in the vitreous.
Half-Life: 9 days, with sustained intraocular activity over 30 days.
Pharmacodynamics of Ranibizumab
This drug exerts its effects by:
- Binding all isoforms of VEGF-A, inhibiting angiogenesis and vascular leakage in the retina.
- Reducing macular edema and stabilizing CNV in wet AMD and DME.
- Demonstrating dose-dependent efficacy with monthly or PRN dosing.
- Exhibiting potential systemic effects with repeated injections, though rare.
Storage of Ranibizumab
Temperature: Store at 2–8°C (36–46°F); do not freeze or shake.
Protection: Keep in original carton to protect from light.
Safety: Store in a locked refrigerator out of reach of children due to injection risk.
Disposal: Dispose of unused vials per biohazard regulations or consult a pharmacist.
Frequently Asked Questions (FAQs)
Q: What does Ranibizumab treat?
A: This medication treats wet AMD and diabetic macular edema.
Q: Can this active ingredient cause eye pain?
A: Yes, eye pain may occur post-injection; report if severe.
Q: Is Ranibizumab safe for children?
A: Yes, for off-label ROP use with a doctor’s guidance.
Q: How is this drug taken?
A: Via intravitreal injection by an ophthalmologist, as directed.
Q: How long is Ranibizumab treatment?
A: Long-term, based on retinal condition and response.
Q: Can I use Ranibizumab if pregnant?
A: Yes, with caution; consult a doctor.
Regulatory Information
This medication is approved by:
U.S. Food and Drug Administration (FDA): Approved in 2006 (Lucentis) for wet AMD, later expanded to DME, RVO, and mCNV.
European Medicines Agency (EMA): Approved for retinal conditions including AMD, DME, and RVO.
Other Agencies: Approved globally for ophthalmic use; consult local guidelines.
References
- U.S. Food and Drug Administration (FDA). (2025). Lucentis (Ranibizumab) Prescribing Information.
- Official FDA documentation detailing the drug’s approved uses, dosage, and safety.
- European Medicines Agency (EMA). (2025). Ranibizumab Summary of Product Characteristics.
- EMA’s comprehensive information on the medication’s indications and precautions in Europe.
- National Institutes of Health (NIH). (2025). Ranibizumab: MedlinePlus Drug Information.
- NIH resource providing detailed information on the drug’s uses, side effects, and precautions.
- World Health Organization (WHO). (2025). WHO Guidelines on Eye Care: Ranibizumab.
- WHO’s recommendations for Ranibizumab in retinal disorders.
- Ophthalmology. (2024). Ranibizumab in Diabetic Retinopathy.
- Peer-reviewed article on Ranibizumab efficacy (note: access may require a subscription).
