Comprehensive Guide to Quinidine: Uses, Dosage, Side Effects, and More
What is Quinidine?
Overview of Quinidine
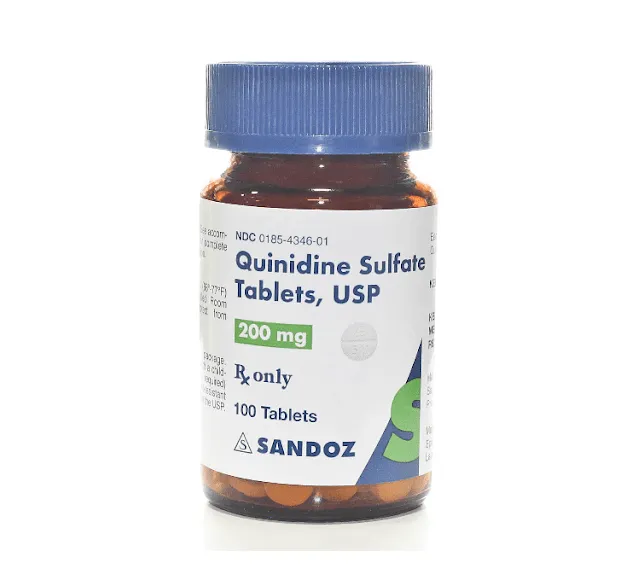
Generic Name: Quinidine
Brand Name: Quinidex, Cardioquin, generics
Drug Group: Class IA antiarrhythmic
Commonly Used For
- Treat atrial fibrillation and flutter.
- Manage ventricular arrhythmias.
- Control malaria (historical use).
Key Characteristics
Form: Oral tablets (200 mg, 300 mg), extended-release tablets (324 mg), or injectable solution (80 mg/mL) (detailed in Dosage section).
Mechanism: Prolongs action potential and refractory period by sodium channel blockade.
Approval: FDA-approved (long-standing use since the 1920s) and EMA-approved for arrhythmias.
Indications and Uses of Quinidine
Quinidine is indicated for cardiac rhythm management, with applications rooted in its historical and modern therapeutic roles:
Atrial Fibrillation (AF): Converts and maintains sinus rhythm in AF, often as a first-line therapy or after cardioversion, supported by cardiology guidelines like those from the AHA/ACC.
Atrial Flutter: Controls atrial flutter by restoring normal rhythm, used in acute or chronic settings, with evidence from electrophysiology studies.
Ventricular Tachycardia (VT): Treats sustained VT in patients without structural heart disease, reducing arrhythmic events, per clinical trial data.
Brugada Syndrome: Used off-label to manage Brugada syndrome-related arrhythmias, stabilizing electrical activity, supported by cardiac genetics research.
Short QT Syndrome: Investigated off-label to prolong QT interval in short QT syndrome, preventing sudden cardiac death, with emerging cardiology evidence.
Malaria (Historical): Formerly used as an antimalarial (replaced by chloroquine), still noted in tropical medicine archives for its cinchona origin.
Myotonic Dystrophy: Explored off-label to reduce cardiac conduction delays in myotonic dystrophy patients, improving quality of life, supported by neuromuscular studies.
Post-Cardiac Surgery Arrhythmias: Managed off-label to control postoperative AF or VT, enhancing recovery, with data from cardiothoracic surgery research.
Long QT Syndrome (Type 3): Investigated off-label to modulate sodium channels in LQT3, reducing arrhythmic risk, noted in genetic cardiology literature.
Dosage of Quinidine
Dosage for Adults
Atrial Fibrillation/Flutter:
- Oral: 200–400 mg every 6 hours or 300–600 mg extended-release every 8–12 hours, titrated to effect.
- IV: 0.25–0.5 mg/kg over 10–15 minutes, followed by infusion if needed.
Ventricular Tachycardia:
- Oral: 200–300 mg every 6 hours, adjusted based on ECG and tolerance.
- IV: 0.25 mg/kg bolus, then 10–20 mcg/kg/min infusion under monitoring.
Dosage for Children
Arrhythmias:
- Oral: 6–10 mg/kg/day divided every 6 hours, titrated under pediatric cardiologist supervision.
- IV: 2–5 mg/kg over 10–15 minutes, with careful monitoring.
- Not recommended under 1 year unless critical.
Dosage for Pregnant Women
Pregnancy Category C: Use only if benefits outweigh risks (e.g., life-threatening arrhythmia). Consult an obstetrician, with fetal monitoring.
Dosage Adjustments
Renal Impairment: Reduce dose by 25–50% if CrCl <50 mL/min; avoid in severe cases.
Hepatic Impairment: Reduce dose by 50% if liver function is compromised; monitor closely.
Elderly: Start with 100–200 mg every 6 hours; increase cautiously with ECG monitoring.
Concomitant Medications: Adjust if combined with CYP3A4 inhibitors/inducers (e.g., verapamil, rifampin), altering levels.
Additional Considerations
- Take this active ingredient with food to minimize gastrointestinal irritation.
- Monitor ECG and serum levels (therapeutic range: 2–5 mg/L).
How to Use Quinidine
Administration:
Swallow tablets whole with food and water; avoid crushing extended-release forms.
IV administration requires slow infusion with ECG monitoring; avoid rapid bolus.
Timing: Use every 6–12 hours (oral) or as directed (IV), maintaining consistency.
Monitoring: Watch for tinnitus, blurred vision, or signs of arrhythmia (e.g., palpitations).
Additional Tips:
- Store at 20–25°C (68–77°F), protecting from moisture and light.
- Keep out of reach of children due to overdose risk.
- Report severe dizziness, hearing changes, or signs of allergic reaction immediately.
Contraindications for Quinidine
Hypersensitivity: Patients with a known allergy to Quinidine or cinchona derivatives.
Complete AV Block: Contraindicated without a pacemaker due to risk of asystole.
Myasthenia Gravis: Avoid due to neuromuscular blockade risk.
Severe Hepatic/Renal Impairment: Contraindicated in advanced disease.
Side Effects of Quinidine
Common Side Effects
- Tinnitus (10–20%, manageable with dose reduction)
- Nausea (8–15%, relieved with food)
- Diarrhea (5–12%, transient)
- Headache (4–10%, relieved with rest)
- Blurred Vision (3–8%, decreases with tolerance)
These effects may subside with dose adjustment.
Serious Side Effects
Seek immediate medical attention for:
- Cardiac: Torsades de pointes, ventricular fibrillation, or asystole.
- Hematologic: Thrombocytopenia or agranulocytosis.
- Gastrointestinal: Severe vomiting or hepatic injury.
- Neurological: Confusion, seizures, or respiratory depression.
- Allergic: Rash, angioedema, or anaphylaxis.
Additional Notes
- Regular monitoring for ECG, blood counts, and liver function is advised.
- Report any unusual symptoms (e.g., irregular heartbeat, yellow skin) immediately to a healthcare provider.
Warnings & Precautions for Quinidine
General Warnings
Proarrhythmic Effects: Risk of torsades de pointes; monitor ECG continuously.
Cinchonism: Symptoms like tinnitus and visual disturbances; reduce dose if present.
Thrombocytopenia: Risk of immune-mediated platelet reduction; check counts.
Hypotension: May occur with rapid IV use; administer slowly.
Drug-Induced Lupus: Rare risk with long-term use; monitor for symptoms.
Additional Warnings
Heart Failure: Worsening in patients with decompensated heart failure; use cautiously.
Hypoglycemia: Rare risk in diabetic patients; monitor glucose.
Respiratory Depression: Risk with overdose or in vulnerable patients; ventilate if needed.
Electrolyte Imbalance: Potentiates toxicity if potassium or magnesium is low; correct levels.
Hypersensitivity Reactions: Rare anaphylaxis; discontinue if swelling occurs.
Use in Specific Populations
- Pregnancy: Category C; use only if essential with fetal monitoring.
- Breastfeeding: Excreted in breast milk; monitor infant for effects.
- Elderly: Higher risk of toxicity; start with lower doses.
- Children: Limited to 1+ years; supervise closely.
- Renal/Hepatic Impairment: Adjust dose; avoid in severe cases.
Additional Precautions
- Inform your doctor about heart disease, electrolyte imbalances, or medication history before starting this medication.
- Avoid abrupt cessation; taper if discontinuing long-term therapy.
Overdose and Management of Quinidine
Overdose Symptoms
- Tinnitus, blurred vision, or confusion (cinchonism).
- Severe cases: Torsades de pointes, hypotension, or respiratory arrest.
- Nausea, vomiting, or dizziness as early signs.
- Cardiac arrest with extremely high doses.
Immediate Actions
Contact the Medical Team: Seek immediate medical help.
Supportive Care: Administer activated charcoal if ingested recently, monitor vital signs, and provide IV fluids or vasopressors.
Specific Treatment: Use sodium bicarbonate for QRS widening, magnesium sulfate for torsades, and dialysis if severe.
Monitor: Check ECG, serum levels, and electrolytes for 24–48 hours.
Additional Notes
- Overdose risk is high; store securely.
- Report persistent symptoms (e.g., severe weakness, irregular heartbeat) promptly.
Drug Interactions with Quinidine
This active ingredient may interact with:
- CYP3A4 Inhibitors/Inducers: Alters levels (e.g., ketoconazole, rifampin); adjust dose.
- Digoxin: Increases digoxin levels; monitor closely.
- Warfarin: Enhances bleeding risk; monitor INR.
- Beta-Blockers: Potentiates bradycardia; use cautiously.
- Antihistamines: Increases QT prolongation risk (e.g., diphenhydramine); avoid.
Action: Provide your healthcare provider with a complete list of medications.
Patient Education or Lifestyle
Medication Adherence: Take this antiarrhythmic as prescribed to manage arrhythmias, following the exact schedule.
Monitoring: Report tinnitus, dizziness, or palpitations immediately.
Lifestyle: Avoid alcohol; limit caffeine to prevent rhythm disturbances.
Diet: Take with food to reduce GI upset; avoid grapefruit juice.
Emergency Awareness: Know signs of arrhythmia or overdose (e.g., fainting); seek care if present.
Follow-Up: Schedule regular check-ups every 1–3 months to monitor ECG, electrolytes, and liver function.
Pharmacokinetics of Quinidine
Absorption: Well-absorbed orally (peak at 1–3 hours); enhanced with food.
Distribution: Volume of distribution ~2.5–3.5 L/kg; 80–90% protein-bound.
Metabolism: Hepatic via CYP3A4 to 3-hydroxyquinidine (active metabolite).
Excretion: Primarily renal (60–80%) as unchanged drug and metabolites; half-life 6–8 hours.
Half-Life: 6–8 hours, prolonged in renal/hepatic impairment.
Pharmacodynamics of Quinidine
This drug exerts its effects by:
- Blocking sodium channels, prolonging phase 0 depolarization in cardiac cells.
- Inhibiting potassium channels, extending action potential duration.
- Reducing ectopic pacemaker activity in arrhythmias.
- Exhibiting dose-dependent proarrhythmic and anticholinergic effects.
Storage of Quinidine
Temperature: Store at 20–25°C (68–77°F); protect from moisture and light.
Protection: Keep in original container, away from heat sources.
Safety: Store in a locked container out of reach of children due to overdose risk.
Disposal: Dispose of unused tablets or vials per local regulations or consult a pharmacist.
Frequently Asked Questions (FAQs)
Q: What does Quinidine treat?
A: This medication treats atrial fibrillation and ventricular tachycardia.
Q: Can this active ingredient cause tinnitus?
A: Yes, tinnitus may occur; report if persistent.
Q: Is Quinidine safe for children?
A: Yes, for 1+ years with a doctor’s guidance.
Q: How is this drug taken?
A: Orally as tablets or via IV, as directed.
Q: How long is Quinidine treatment?
A: Varies by condition, often long-term with monitoring.
Q: Can I use Quinidine if pregnant?
A: Yes, with caution; consult a doctor.
Regulatory Information
This medication is approved by:
U.S. Food and Drug Administration (FDA): Approved since the 1920s, with updated indications for arrhythmias.
European Medicines Agency (EMA): Approved for cardiac rhythm management.
Other Agencies: Approved globally for arrhythmias; consult local guidelines.
References
- U.S. Food and Drug Administration (FDA). (2023). Quinidine Prescribing Information.
- Official FDA documentation detailing the drug’s approved uses, dosage, and safety.
- European Medicines Agency (EMA). (2023). Quinidine Summary of Product Characteristics.
- EMA’s comprehensive information on the medication’s indications and precautions in Europe.
- National Institutes of Health (NIH). (2023). Quinidine: MedlinePlus Drug Information.
- NIH resource providing detailed information on the drug’s uses, side effects, and precautions.
- American Heart Association (AHA). (2023). AHA/ACC Guidelines on Arrhythmias.
- AHA guidelines including Quinidine use in arrhythmia management.
- Journal of the American College of Cardiology. (2022). Quinidine in Rare Arrhythmias.
- Peer-reviewed article on Quinidine efficacy (note: access may require a subscription).
