Multifocal Breast Cancer: Causes, Symptoms, and Treatment
Overview of Multifocal Breast Cancer
What is Multifocal Breast Cancer?
Multifocal breast cancer refers to the presence of two or more malignant lesions arising within the same breast quadrant or region, typically stemming from a single primary tumor.
It must be differentiated from multicentric breast cancer, where multiple tumors arise independently in different quadrants of the breast.
Depending on diagnostic criteria, multifocal breast cancer accounts for 10–60% of breast cancer cases.
It is not necessarily more invasive than other subtypes; prognosis largely depends on the features of the largest primary tumor. However, multifocal disease is associated with higher recurrence and metastasis rates, potentially impacting outcomes.
Non-Invasive Breast Cancer
Also known as carcinoma in situ, this type remains confined to its original location without invasion of surrounding tissue. It has not extended beyond the epithelial lining of the ducts or lobules.
Ductal Carcinoma In Situ (DCIS): Begins within the breast ducts and is considered non-invasive. DCIS increases the likelihood of developing invasive breast cancer later.
Lobular Carcinoma In Situ (LCIS): Not considered a true cancer but reflects atypical cell changes in the lobules. According to the American Cancer Society, individuals with LCIS have a 7–12 times higher risk of developing invasive breast cancer in either breast.
Invasive Breast Cancer
This form invades nearby breast tissue and may spread to other parts of the body. Two major invasive types include:
Invasive Ductal Carcinoma (IDC): The most common type, accounting for ~80% of breast cancer diagnoses in the United States. It begins in the ducts and invades the surrounding breast tissue.
Invasive Lobular Carcinoma (ILC): Arises in the lobules and spreads into adjacent breast tissue. It represents about 10% of invasive breast cancers.

Symptoms of Multifocal Breast Cancer
Typical local changes include:
- Breast swelling or lumps;
- Skin dimpling or puckering;
- Breast pain or tenderness;
- Nipple inversion;
- Redness, itchiness, flaking, or irritation of the breast skin;
- Nipple discharge (yellowish, purulent, thick or thin fluid).
Systemic symptoms may include:
- Persistent fatigue;
- Bone pain (suggesting bone metastases);
- Unexplained weight loss;
- Nausea or loss of appetite;
- Jaundice (if liver metastases);
- Shortness of breath or cough;
- Headaches or double vision.

Complications
Compared to unifocal breast cancer, multifocal disease may have a higher risk of local recurrence.
A 2019 meta-analysis of 17 comparative studies and 7 case series (3,537 patients undergoing breast-conserving surgery) reported local recurrence rates ranging from 2–23% over a mean follow-up of 59.5 months—comparable to mastectomy outcomes, but further studies are needed.
Five-year relative survival rates (American Cancer Society):
- Localized (no spread): 99%
- Regional (spread to nearby structures or lymph nodes): 86%
- Distant metastases: 31%
- Overall (all stages): 91%
Prognosis depends on:
- Age;
- Overall health;
- Tumor size;
- Response to therapy;
- Presence of metastasis.
When to See a Doctor
Seek prompt evaluation if you notice:
- New lumps or persistent breast pain/swelling;
- Nipple inversion or abnormal discharge (yellow, bloody, or purulent);
- Persistent redness, flaking, or irritation;
- Unexplained fatigue or weight loss;
- Personal or family history of breast cancer.

Causes
The exact mechanism of uncontrolled breast cell growth remains under investigation, but genetic mutations and lifestyle factors play key roles. Mutations may disrupt DNA repair signals, allowing unchecked cell proliferation:
BRCA1 and BRCA2 mutations: These genes produce proteins critical for DNA repair. Mutations lead to defective repair and abnormal cell growth. Women carrying these mutations face a lifetime breast cancer risk of 50–85% (compared to 12% in the general population). BRCA mutations also elevate ovarian cancer risk. Men with BRCA mutations are also at higher risk for breast and other cancers.
Family history: Even without BRCA mutations, risk increases if a mother, sister, or daughter developed breast cancer before age 40, if two relatives developed it before age 50, or if male relatives developed breast cancer. Multiple affected relatives or a history of both breast and ovarian cancer further elevates risk.
Risk Factors
Younger age: Multifocal breast cancer tends to be diagnosed in younger women.
Family history: Especially if multiple relatives are affected or bilateral breast cancer is present.
Genetic predisposition: BRCA1/BRCA2 and other related mutations.
Lifestyle: Alcohol use, smoking, poor diet, and prolonged hormone replacement therapy.
Medical history: Previous breast cancer or chest radiation.
Environmental exposure: Long-term contact with carcinogenic substances.

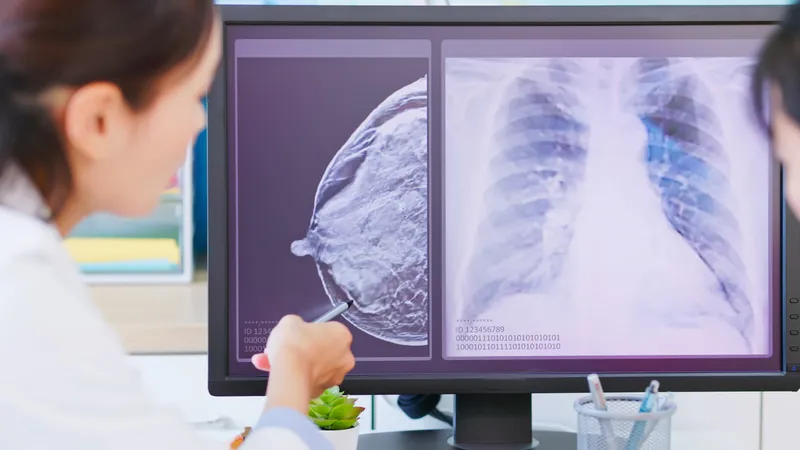
Diagnosis
Physicians perform a comprehensive breast exam to detect abnormalities. Key tests include:
- Mammography: X-ray imaging for screening and diagnosis.
- Breast ultrasound: Uses sound waves to evaluate internal structures.
- Breast MRI: Provides high-resolution imaging of soft tissue for improved accuracy.
- Biopsy: Sampling of tissue or fluid to confirm malignancy.
- Genetic blood testing: Detects mutations associated with breast cancer.
Treatment
Therapy depends on stage, age, health status, and metastasis:
Surgery:
Lumpectomy: Removal of tumors with surrounding normal tissue, often preferred for lesions <5 cm.
Mastectomy: Complete removal of breast tissue with lymph node dissection to reduce recurrence risk.
Possible side effects: Cosmetic changes, pain, scarring, infection, or swelling.
Radiotherapy:
High-dose radiation to destroy residual cancer cells after surgery.
Side effects: Pain, swelling, skin redness, fatigue, sore throat, or lymphedema.
Chemotherapy:
Systemic therapy targeting rapidly dividing cancer cells, administered before or after surgery.
Side effects: Hair loss, nausea, diarrhea, increased infection and bleeding risk.

Lifestyle and Prevention
Healthy Habits:
Regular follow-up: Adhere to checkups and monitoring schedules; report new symptoms promptly.
Physical activity: Gentle exercise such as yoga, walking, or swimming can boost well-being. Consult your physician before starting.
Mental health: Join cancer support groups and continue enjoyable activities to reduce stress.
Skin care: Avoid direct sun on irradiated skin; use gentle, non-irritating products.
Nutrition:
Recommended:
- Leafy greens, tomatoes, broccoli, and berries rich in antioxidants;
- Protein sources such as fish, eggs, tofu, and chicken to support energy and recovery;
- Whole grains like brown rice and oats for fiber;
- Hydration: 2–3 liters of water daily, plus green tea or unsweetened juices.
Limit:
- Processed, high-fat, or sugary foods;
- Alcohol and caffeine.

Prevention:
Screening: Mammograms, ultrasound, or genetic testing if high-risk.
Maintain healthy weight: Avoid overweight/obesity.
No smoking; limit alcohol: Both linked to higher breast cancer risk.
Balanced diet: Prioritize vegetables and fruits, limit processed food.
Exercise regularly: At least 30 minutes per day.
Reduce carcinogen exposure: Avoid harmful chemicals at work or in the environment.
Manage comorbidities: Control diabetes, hypertension, and hormone-related disorders.
