Comprehensive Guide to Epinephrine: Uses, Dosage, Side Effects, and More
What is Epinephrine?
Overview of Epinephrine
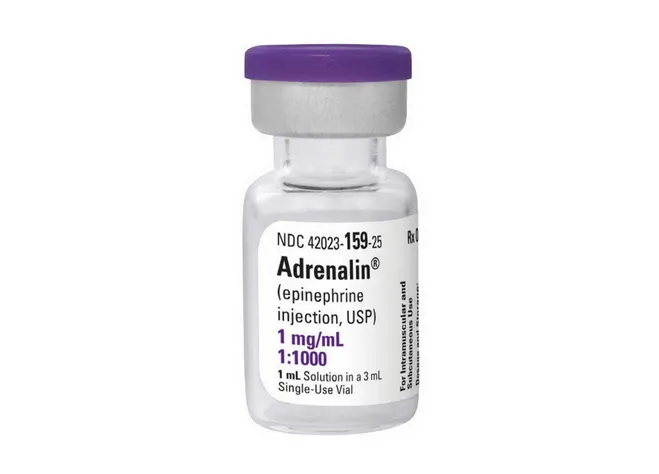
Generic Name: Epinephrine
Brand Name: EpiPen, Adrenalin, generics
Drug Group: Catecholamine (vasopressor, bronchodilator, cardiac stimulant)
Commonly Used For
- Treat anaphylaxis and allergic emergencies.
- Manage cardiac arrest.
- Relieve severe asthma attacks.
Key Characteristics
Form: Auto-injectors (0.3 mg, 0.15 mg), vials for injection (1 mg/mL), inhalation solutions, or topical preparations (detailed in Dosage section).
Mechanism: Activates adrenergic receptors, increasing heart rate and bronchodilation.
Approval: FDA-approved (1938 for Adrenalin) and EMA-approved for emergency use.
Indications and Uses of Epinephrine
Epinephrine is indicated for a range of acute and emergency conditions, leveraging its sympathomimetic effects:
Anaphylaxis: Reverses life-threatening allergic reactions, per allergy guidelines, supported by clinical trials.
Cardiac Arrest: Restores circulation during resuscitation, improving survival rates, recommended in cardiology protocols.
Severe Asthma: Relieves acute bronchospasm, enhancing airflow, with pulmonary medicine evidence.
Anaphylactoid Reactions: Manages non-immune hypersensitivity, reducing symptoms, per emergency medicine studies.
Septic Shock: Supports hemodynamic stability, increasing blood pressure, with critical care research.
Croup: Investigated off-label to reduce airway swelling in children, with pediatric otolaryngology data.
Local Anesthesia Adjunct: Used off-label with lidocaine to prolong effects, with anesthesiology evidence.
Hypotensive Emergencies: Explored off-label to treat profound hypotension, with emergency medicine studies.
Glaucoma (Topical): Managed off-label to reduce intraocular pressure, with ophthalmology research.
Priapism: Initiated off-label to reverse prolonged erection, with urology data.
Dosage of Epinephrine
Dosage for Adults
Anaphylaxis:
- IM (Auto-injector): 0.3–0.5 mg (EpiPen) into the thigh, repeat every 5–15 minutes if needed.
- IV: 0.1–0.5 mg every 5 minutes during resuscitation.
Cardiac Arrest:
- IV/IO: 1 mg every 3–5 minutes during CPR.
Severe Asthma:
- Subcutaneous: 0.1–0.5 mg every 20 minutes for 3 doses.
Dosage for Children
Anaphylaxis:
- IM: 0.01 mg/kg (max 0.3 mg) using EpiPen Jr. or vial, repeat if needed, under pediatric supervision.
Cardiac Arrest:
- IV/IO: 0.01 mg/kg every 3–5 minutes (max 1 mg).
Dosage for Pregnant Women
Pregnancy Category C: Use only if benefits outweigh risks; consult an obstetrician, with fetal monitoring.
Dosage Adjustments
Renal Impairment: No adjustment needed; monitor in severe cases.
Hepatic Impairment: Mild to moderate (Child-Pugh A or B): Use cautiously; severe (Child-Pugh C): Avoid.
Concomitant Medications: Adjust if combined with beta-blockers, reducing efficacy; monitor response.
Elderly: Start with lower doses; monitor for hypertension.
Additional Considerations
- Administer this active ingredient via IM injection into the outer thigh, avoiding veins.
- Use auto-injectors for rapid self-administration in emergencies.
How to Use Epinephrine
Administration:
IM: Inject into the anterolateral thigh using an auto-injector or syringe.
IV: Administer slowly under medical supervision.
Inhalation: Use nebulized solution for asthma, following provider guidance.
Timing: Administer immediately in emergencies, repeating as directed.
Monitoring: Watch for palpitations, chest pain, or signs of overdose (e.g., tremor).
Additional Tips:
- Store at 20–25°C (68–77°F), protecting from light and freezing.
- Keep out of reach of children; check expiration dates on auto-injectors.
- Report severe headache, shortness of breath, or signs of allergic reactions immediately.
Contraindications for Epinephrine
Hypersensitivity: Patients with a known allergy to Epinephrine or sulfites.
Angle-Closure Glaucoma: Avoid due to increased intraocular pressure.
Severe Hypertension: Contraindicated in uncontrolled high blood pressure.
Cardiomyopathy: Avoid in hypertrophic obstructive cardiomyopathy.
Concurrent Use with Non-Selective Beta-Blockers: Avoid due to paradoxical effects.
Warnings & Precautions for Epinephrine
General Warnings
Cardiac Arrhythmias: Risk of tachycardia or ventricular fibrillation; monitor ECG.
Hypertension: Risk of severe blood pressure elevation; assess regularly.
Pulmonary Edema: Risk in heart failure patients; monitor respiratory status.
Hypokalemia: Risk with repeated doses; check potassium levels.
Necrosis: Risk with extravasation during IV use; use with care.
Additional Warnings
Cerebral Hemorrhage: Rare risk; monitor in stroke-prone patients.
Hyperglycemia: Risk in diabetic patients; monitor glucose.
Anxiety/Agitation: Common side effect; reassure patient.
Renal Impairment: Risk of toxicity; monitor renal function.
Hypersensitivity Reactions: Rare anaphylaxis; discontinue if severe.
Use in Specific Populations
Pregnancy: Category C; use with caution and monitoring.
Breastfeeding: Use caution; monitor infant for effects.
Elderly: Higher risk of cardiovascular events; start low and monitor.
Children: Safe for anaphylaxis with supervision.
Renal/Hepatic Impairment: Adjust or avoid in severe cases.
Additional Precautions
- Inform your doctor about heart disease, diabetes, or thyroid issues before starting this medication.
- Avoid overuse to prevent cardiovascular strain.
Overdose and Management of Epinephrine
Overdose Symptoms
- Palpitations, anxiety, or headache.
- Severe cases: Cardiac arrest, pulmonary edema, or cerebral hemorrhage.
- Tremors, sweating, or nausea as early signs.
- Coma or profound hypotension with extremely high doses.
Immediate Actions
Contact the Medical Team: Seek immediate medical help.
Supportive Care: Monitor vital signs, provide oxygen, and manage arrhythmias with beta-blockers if needed.
Specific Treatment: No specific antidote; use phentolamine for extravasation.
Monitor: Check ECG, blood pressure, and glucose for 24–48 hours.
Additional Notes
- Overdose risk is significant in non-emergency use; store securely and limit access.
- Report persistent symptoms (e.g., chest pain, severe headache) promptly.
Side Effects of Epinephrine
Common Side Effects
- Palpitations (20–30%, decreases with time)
- Anxiety (15–25%, managed with reassurance)
- Tremors (10–20%, reduced with rest)
- Headache (10–15%, relieved with hydration)
- Nausea (5–10%, controlled with food)
These effects may subside with adaptation.
Serious Side Effects
Seek immediate medical attention for:
- Cardiac: Arrhythmias or myocardial infarction.
- Neurological: Cerebral hemorrhage or seizures.
- Pulmonary: Pulmonary edema or bronchospasm.
- Metabolic: Severe hyperglycemia or lactic acidosis.
- Allergic: Rash, angioedema, or anaphylaxis.
Additional Notes
- Regular monitoring for cardiac rhythm, blood pressure, and glucose is advised.
- Report any unusual symptoms (e.g., irregular heartbeat, shortness of breath) immediately to a healthcare provider.
Drug Interactions with Epinephrine
This active ingredient may interact with:
- Beta-Blockers: Reduces efficacy (e.g., propranolol); monitor response.
- Tricyclic Antidepressants: Increases pressor effects; adjust dose.
- MAOIs: Enhances hypertensive risk; avoid within 14 days.
- Diuretics: Potentiates hypokalemia; monitor electrolytes.
- Levothyroxine: Amplifies cardiovascular effects; use cautiously.
Action: Provide your healthcare provider with a complete list of medications.
Patient Education or Lifestyle
Medication Adherence: Use this catecholamine as prescribed for emergencies, following auto-injector instructions.
Monitoring: Report palpitations, anxiety, or signs of overdose immediately.
Lifestyle: Avoid stimulants (e.g., caffeine); maintain calm during use.
Diet: No specific restrictions; take with water if oral.
Emergency Awareness: Know signs of cardiac distress or allergic reaction; seek care if present.
Follow-Up: Schedule regular check-ups post-use to monitor cardiac and metabolic health.
Pharmacokinetics of Epinephrine
Absorption: Rapid via IM (peak at 5–10 minutes); IV immediate; bioavailability ~30% (oral, degraded).
Distribution: Volume of distribution ~0.2 L/kg; 50% protein-bound.
Metabolism: Hepatic and plasma via COMT and MAO to metanephrine and vanillylmandelic acid.
Excretion: Primarily renal (as metabolites); half-life 2–3 minutes.
Half-Life: 2–3 minutes, with prolonged effects due to receptor binding.
Pharmacodynamics of Epinephrine
This drug exerts its effects by:
Stimulating alpha-1 receptors for vasoconstriction and beta-2 receptors for bronchodilation.
Increasing cardiac output via beta-1 stimulation during arrest.
Reversing anaphylaxis by counteracting histamine effects.
Exhibiting dose-dependent risks of arrhythmias and hypertension.
Storage of Epinephrine
- Temperature: Store at 20–25°C (68–77°F); protect from light and freezing (auto-injectors at 15–30°C).
- Protection: Keep in original packaging, away from heat and humidity.
- Safety: Store in a secure, accessible location out of reach of children for emergencies.
- Disposal: Dispose of expired auto-injectors or vials per local regulations or consult a pharmacist.
Frequently Asked Questions (FAQs)
Q: What does Epinephrine treat?
A: This medication treats anaphylaxis and cardiac arrest.
Q: Can this active ingredient cause palpitations?
A: Yes, palpitations are common; monitor closely.
Q: Is Epinephrine safe for children?
A: Yes, for anaphylaxis with supervision.
Q: How is this drug taken?
A: Via IM injection, IV, or inhalation, as directed.
Q: How long is Epinephrine effective?
A: Effects are immediate, lasting 5–20 minutes.
Q: Can I use Epinephrine if pregnant?
A: Yes, with caution; consult a doctor.
Regulatory Information
This medication is approved by:
U.S. Food and Drug Administration (FDA): Approved in 1938 (Adrenalin) for emergency use.
European Medicines Agency (EMA): Approved for anaphylaxis, cardiac arrest, and asthma.
Other Agencies: Approved globally for emergency therapy; consult local guidelines.
References
- U.S. Food and Drug Administration (FDA). (2023). Adrenalin (Epinephrine) Prescribing Information.
- Official FDA documentation detailing the drug’s approved uses, dosage, and safety.
- European Medicines Agency (EMA). (2023). Epinephrine Summary of Product Characteristics.
- EMA’s comprehensive information on the medication’s indications and precautions in Europe.
- National Institutes of Health (NIH). (2023). Epinephrine: MedlinePlus Drug Information.
- NIH resource providing detailed information on the drug’s uses, side effects, and precautions.
- World Health Organization (WHO). (2023). WHO Model List of Essential Medicines: Epinephrine.
- WHO’s inclusion of Epinephrine for emergency use.
- Journal of Allergy and Clinical Immunology. (2022). Epinephrine in Anaphylaxis.
- Peer-reviewed article on Epinephrine efficacy (note: access may require a subscription).
