Comprehensive Guide to Mebendazole: Uses, Dosage, Side Effects, and More
What is Mebendazole?
Overview of Mebendazole
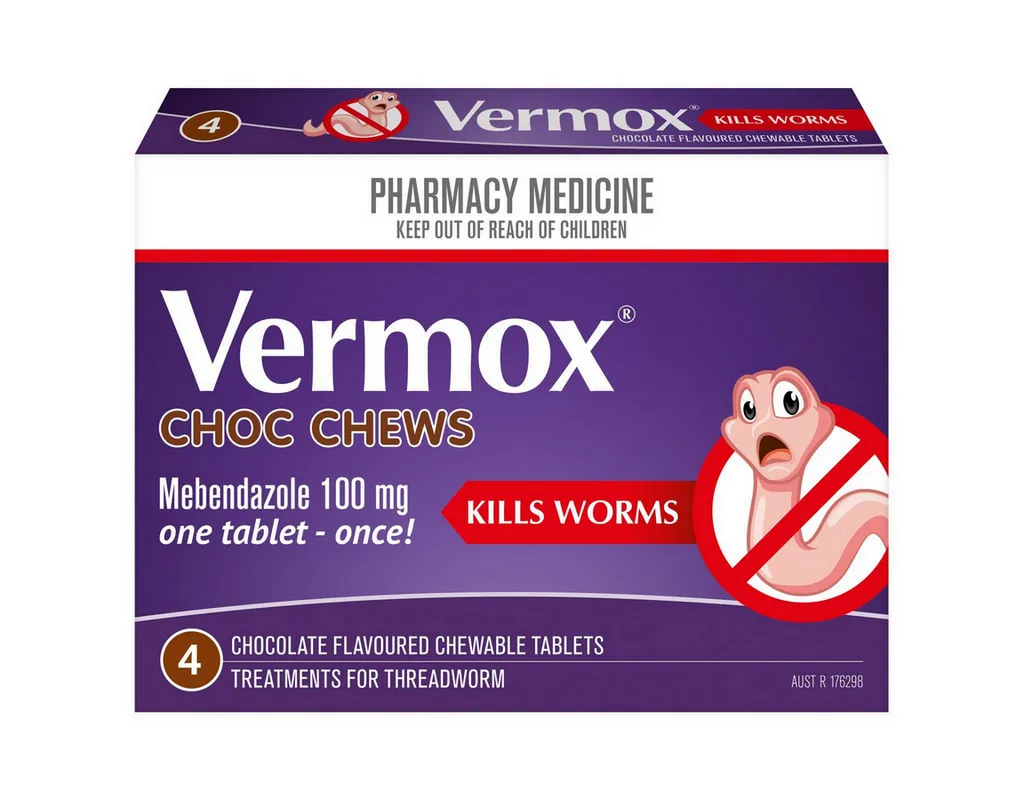
Generic Name: Mebendazole
Brand Name: Vermox, Emverm, generics
Drug Group: Anthelmintic (anti-parasitic)
Commonly Used For
- Treat pinworm infections.
- Manage roundworm infections.
- Eradicate whipworm infections.
Key Characteristics
Form: Oral tablets (100 mg), chewable tablets (100 mg), or oral suspension (20 mg/mL) (detailed in Dosage section).
Mechanism: Inhibits microtubule formation in parasites, causing energy depletion.
Approval: FDA-approved (1971 for Vermox) and EMA-approved for parasitic infections.
Indications and Uses of Mebendazole
Mebendazole is indicated for a variety of parasitic infections, leveraging its broad-spectrum anthelmintic activity:
Enterobiasis (Pinworm Infection): Eliminates Enterobius vermicularis, reducing anal itching and transmission, per parasitology guidelines, supported by clinical trials showing 90–100% efficacy within 7 days.
Ascariasis (Roundworm Infection): Treats Ascaris lumbricoides, preventing intestinal obstruction, recommended in tropical medicine protocols with evidence of worm expulsion within 3–7 days.
Trichuriasis (Whipworm Infection): Manages Trichuris trichiura, alleviating abdominal pain, with gastroenterology data.
Hookworm Infections: Eradicates Ancylostoma duodenale and Necator americanus, improving nutritional status, per infectious disease studies.
Strongyloidiasis: Investigated off-label to treat Strongyloides stercoralis, reducing larval migration, with parasitology research.
Taeniasis (Tapeworm Infection): Used off-label against Taenia species, expelling segments, with helminthology evidence.
Hydatid Disease (Off-Label): Explored as an adjunct to surgery for Echinococcus granulosus, with surgical-parasitic studies.
Trichinellosis: Managed off-label in severe cases of Trichinella spiralis, reducing muscle inflammation, with infectious disease data.
Giardiasis (Off-Label): Investigated for Giardia lamblia in resistant cases, with gastroenterology research.
Cutaneous Larva Migrans: Initiated off-label to treat Ancylostoma braziliense, with dermatology-parasitology evidence.
Dosage of Mebendazole
Dosage for Adults
Enterobiasis (Pinworm): 100 mg as a single dose, repeated after 2 weeks to prevent reinfection.
Ascariasis, Trichuriasis, or Hookworm: 100 mg twice daily for 3 days, or 500 mg as a single dose for light infections.
Mixed Infections: 100 mg twice daily for 3–5 days, depending on parasite load.
Dosage for Children (≥2 years)
Enterobiasis: 100 mg as a single dose, repeated after 2 weeks, under pediatric supervision.
Ascariasis or Trichuriasis: 100 mg twice daily for 3 days (or 500 mg single dose if <10 kg with caution).
Dosage for Pregnant Women
Pregnancy Category C: Use only if benefits outweigh risks; consult an obstetrician, with fetal monitoring and limited to single-dose therapy if necessary.
Dosage Adjustments
Renal Impairment: No adjustment needed; monitor for rare systemic effects.
Hepatic Impairment: Mild to moderate (Child-Pugh A or B): Use cautiously; severe (Child-Pugh C): Avoid due to potential toxicity.
Concomitant Medications: Adjust if combined with CYP450 inducers (e.g., rifampin), reducing efficacy; monitor response.
Elderly: No specific adjustment; assess liver function and nutritional status.
Reinfection Risk: Consider repeat dosing or family prophylaxis for pinworm.
Additional Considerations
- Take this active ingredient with or without food, chewing tablets if necessary or mixing suspension with water.
- Maintain good hygiene (e.g., handwashing, nail trimming) to prevent reinfection.
- Administer to all household members if pinworm is diagnosed.
How to Use Mebendazole
Administration:
- Oral: Swallow tablets whole or chew, or administer suspension with a spoon or syringe, taken with a glass of water.
- Shake suspension well before use; measure with a calibrated device.
Timing: Take as a single dose or twice daily for 3 days, depending on indication, at consistent times.
Monitoring: Watch for abdominal pain, rash, or signs of liver issues (e.g., jaundice); report changes immediately.
Additional Tips:
- Store at 15–30°C (59–86°F), protecting from moisture and light.
- Keep out of reach of children; dispose of unused medication per local regulations.
- Wash bedding and clothing in hot water to prevent reinfection, especially for pinworm.
- Schedule follow-up stool exams 2–3 weeks post-treatment to confirm parasite clearance.
- Educate patients on hygiene practices, including daily bathing and avoiding scratching.
Contraindications for Mebendazole
Hypersensitivity: Patients with a known allergy to Mebendazole or other benzimidazole derivatives.
Severe Hepatic Impairment: Contraindicated in Child-Pugh Class C due to risk of toxicity.
Pregnancy (First Trimester): Avoid unless life-threatening infection, due to teratogenic potential.
Infants <2 Years: Contraindicated due to limited safety data and risk of overdose.
Active Liver Disease: Avoid in acute hepatitis or cirrhosis without specialist oversight.
Crohn’s Disease or Ulcerative Colitis: Contraindicated due to potential exacerbation.
Side Effects of Mebendazole
Common Side Effects
- Abdominal Pain (10–20%, managed with rest)
- Diarrhea (5–15%, controlled with hydration)
- Nausea (5–10%, reduced with food)
- Rash (2–8%, relieved with antihistamines)
- Dizziness (1–5%, decreases with time)
These effects may subside with adaptation.
Serious Side Effects
Seek immediate medical attention for:
- Hepatic: Jaundice, hepatitis, or liver failure.
- Hematologic: Neutropenia, thrombocytopenia, or aplastic anemia.
- Neurological: Seizures or encephalopathy (rare with high doses).
- Gastrointestinal: Severe obstruction or perforation.
- Allergic: Anaphylaxis or Stevens-Johnson syndrome (rare).
Additional Notes
Regular monitoring with liver function tests (LFTs) and CBC every 1–2 weeks is advised during prolonged use (>1 month).
Patients with heavy parasite loads should be monitored for intestinal obstruction, with imaging if severe pain occurs.
Report any unusual symptoms (e.g., persistent fever, dark urine) immediately to a healthcare provider to address potential toxicity.
Long-term use requires bone marrow function assessments and nutritional support to mitigate risks.
Warnings & Precautions for Mebendazole
General Warnings
Liver Toxicity: Risk of elevated liver enzymes or hepatitis; monitor function tests every 1–2 weeks during prolonged use.
Bone Marrow Suppression: Rare risk of neutropenia or thrombocytopenia; check CBC weekly if used >1 month.
Neurotoxicity: Risk of seizures in high doses; avoid in patients with seizure history.
Gastrointestinal Obstruction: Risk if large worm burden dies; monitor for abdominal pain.
Allergic Reactions: Risk of rash or angioedema; discontinue if severe.
Additional Warnings
Malnutrition: Increased toxicity risk in malnourished patients; assess nutritional status.
Reinfection: High risk with poor hygiene; implement family-wide treatment.
Drug Resistance: Emerging resistance in some parasites (e.g., Trichuris); consider alternative therapies.
Renal Impairment: Rare systemic effects; monitor in severe cases.
Hypersensitivity Reactions: Rare anaphylaxis; stop if swelling occurs.
Use in Specific Populations
- Pregnancy: Category C; use with caution, limiting to single doses after first trimester.
- Breastfeeding: Use caution; monitor infant for gastrointestinal effects.
- Elderly: Higher risk of toxicity; start with lower doses and monitor.
- Children: Safe for ≥2 years with supervision.
- Renal/Hepatic Impairment: Avoid or adjust in severe cases.
Additional Precautions
- Inform your doctor about liver disease, pregnancy, or recent surgery before starting this medication.
- Avoid alcohol during therapy to reduce liver strain.
- Use protective measures (e.g., gloves) when handling soiled linens to prevent reinfection.
Overdose and Management of Mebendazole
Overdose Symptoms
- Nausea, vomiting, or abdominal pain.
- Severe cases: Liver failure, neutropenia, or seizures.
- Diarrhea, dizziness, or rash as early signs.
- Coma or profound bone marrow suppression with extremely high doses.
Immediate Actions
Contact the Medical Team: Seek immediate medical help if overdose is suspected.
Supportive Care: Administer activated charcoal if ingestion is recent, monitor liver function, and provide IV fluids if needed.
Specific Treatment: No specific antidote; use granulocyte colony-stimulating factor (G-CSF) for severe neutropenia under specialist guidance.
Monitor: Check liver enzymes, CBC, and neurological status for 24–72 hours.
Patient Education: Advise against self-medicating and to store safely away from children.
Additional Notes
- Overdose risk is low with standard doses; systemic absorption is minimal but increases with overdose.
- Report persistent symptoms (e.g., yellowing skin, severe fatigue) promptly to prevent complications.
Drug Interactions with Mebendazole
This active ingredient may interact with:
- CYP450 Inducers: Reduces efficacy (e.g., carbamazepine, phenytoin); increase dose if needed.
- Cimetidine: Increases levels; monitor for toxicity.
- Anticoagulants: Enhances bleeding risk (e.g., warfarin); check INR.
- Metronidazole: Potentiates gastrointestinal effects; use cautiously.
- Antiepileptics: May alter seizure threshold; monitor.
Action: Provide your healthcare provider with a complete list of medications.
Patient Education or Lifestyle
Medication Adherence: Use this anthelmintic as prescribed for parasitic infections, following the exact schedule.
Monitoring: Report abdominal pain, rash, or signs of liver issues immediately.
Lifestyle: Maintain strict hygiene (e.g., handwashing, cleaning); avoid barefoot walking in endemic areas.
Diet: No specific restrictions; ensure adequate nutrition.
Emergency Awareness: Know signs of overdose or severe reaction; seek care if present.
Follow-Up: Schedule stool exams 2–3 weeks post-treatment and check-ups if symptoms persist.
Pharmacokinetics of Mebendazole
Absorption: Poor oral bioavailability (~5–10%); enhanced with fatty meals; peak at 2–4 hours.
Distribution: Volume of distribution ~1–2 L/kg; 90–95% protein-bound.
Metabolism: Hepatic via CYP450 to active and inactive metabolites.
Excretion: Primarily fecal (via bile, 70–90%); renal (<2%); half-life 3–6 hours.
Half-Life: 3–6 hours, prolonged with liver impairment.
Pharmacodynamics of Mebendazole
This drug exerts its effects by:
- Inhibiting tubulin polymerization in parasitic worms, disrupting microtubule function.
- Depleting glucose stores, leading to immobilization and death of parasites.
- Exhibiting dose-dependent risks of hepatotoxicity and marrow suppression.
Storage of Mebendazole
Temperature: Store at 15–30°C (59–86°F); protect from moisture and light.
Protection: Keep in original container, away from heat and humidity.
Safety: Store in a secure location out of reach of children and pets due to toxicity risk.
Disposal: Dispose of unused tablets or suspension per local regulations or consult a pharmacist.
Frequently Asked Questions (FAQs)
Q: What does Mebendazole treat?
A: This medication treats parasitic worm infections.
Q: Can this active ingredient cause abdominal pain?
A: Yes, abdominal pain is common; report if severe.
Q: Is Mebendazole safe for children?
A: Yes, for ≥2 years with supervision.
Q: How is this drug taken?
A: Orally as tablets or suspension, as directed.
Q: How long is Mebendazole treatment?
A: Typically 1–3 days, with repeat if needed.
Q: Can I use Mebendazole if pregnant?
A: Yes, with caution after first trimester; consult a doctor.
Regulatory Information
This medication is approved by:
U.S. Food and Drug Administration (FDA): Approved in 1971 (Vermox) for parasitic infections.
European Medicines Agency (EMA): Approved for enterobiasis, ascariasis, and trichuriasis.
Other Agencies: Approved globally for anthelmintic therapy; consult local guidelines.
References
- U.S. Food and Drug Administration (FDA). (2023). Vermox (Mebendazole) Prescribing Information.
- Official FDA documentation detailing the drug’s approved uses, dosage, and safety.
- European Medicines Agency (EMA). (2023). Mebendazole Summary of Product Characteristics.
- EMA’s comprehensive information on the medication’s indications and precautions in Europe.
- National Institutes of Health (NIH). (2023). Mebendazole: MedlinePlus Drug Information.
- NIH resource providing detailed information on the drug’s uses, side effects, and precautions.
- World Health Organization (WHO). (2023). WHO Model List of Essential Medicines: Mebendazole.
- WHO’s inclusion of Mebendazole for parasitic infections.
- American Journal of Tropical Medicine and Hygiene. (2022). Mebendazole in Hookworm.
- Peer-reviewed article on Mebendazole efficacy (note: access may require a subscription).
