Perivascular Cell Tumor: Causes, Symptoms, and Treatment
Overview of Perivascular Cell Tumors
What are Perivascular Cell Tumors?
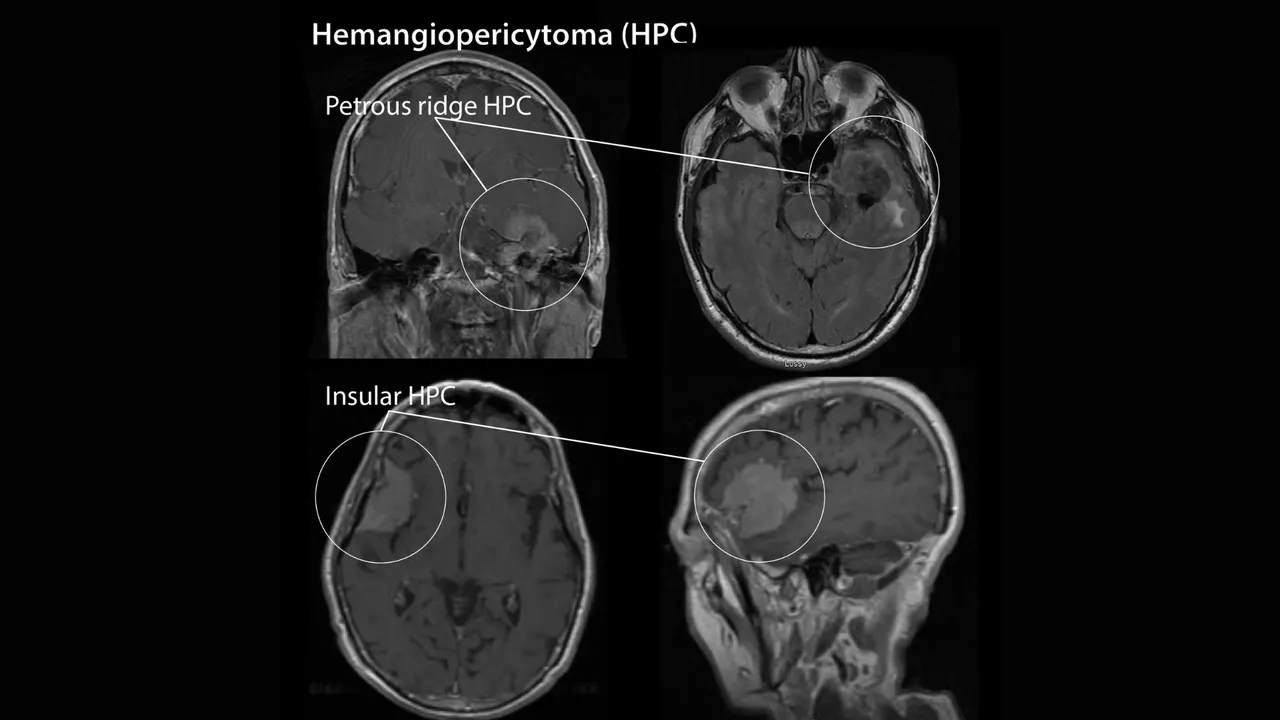
Hemangiopericytoma (HPC) is a tumor that develops from soft tissue and the blood vessels embedded within that tissue. It can arise anywhere in the body where blood vessels are present, though it is most commonly seen in the head and neck, particularly at the skull base.
Perivascular cell tumors may be either benign (non-cancerous) or malignant (cancerous). Malignant tumors have the potential to metastasize, most often spreading to the lungs and bones. When hemangiopericytomas occur in the nasal cavity (glomangiopericytoma) or paranasal sinuses, the prognosis is usually more favorable because these tumors tend to be less invasive and rarely metastasize.
Symptoms of Hemangiopericytoma (Perivascular Cell Tumor)
Hemangiopericytoma often causes no obvious symptoms, especially when the tumor is small. Because the surrounding soft tissue is elastic and can accommodate a slow-growing mass, these tumors may remain unnoticed for a long time. Typical features include:
- Painless mass: Most hemangiopericytomas are painless and may persist for months or years before being detected.
- Swelling or unusual lump: Some patients notice unexplained swelling or a palpable mass in a specific area.
- Pain or pressure: As the tumor enlarges, it can cause localized pain, a sensation of pressure, or swelling around the site.
- Neurological disturbances: Tumors at the skull base may compress nerves, leading to headaches, sensory changes, muscle weakness or paralysis, and even speech difficulties.
- Nasal cavity discomfort: When the tumor arises in the nasal cavity (glomangiopericytoma), patients may experience pain or a sense of blockage in the nose.
If the tumor spreads to the lungs, additional symptoms may occur:
- Persistent cough, sometimes with blood
- Chest pain or tightness
- Shortness of breath
- Night sweats

Complications of Hemangiopericytoma (Perivascular Cell Tumor)
- Local invasion: The tumor can grow large enough to compress surrounding tissues or organs, causing pain, functional limitations, or visible deformity in the affected area.
- Metastasis: In malignant cases, hemangiopericytomas may spread to other organs, most commonly the lungs and bones.
- Neurological impairment: Tumors located at the skull base can damage nerves, leading to sensory loss, reduced vision or hearing, or muscle weakness.
- Organ dysfunction: When the tumor develops in areas such as the nasal cavity or lungs, it may severely impair breathing or cause pronounced nasal obstruction.
- Hypoglycemia: Some tumors may interfere with blood sugar regulation, resulting in persistent low blood glucose levels.
When to See a Doctor
Seek medical care promptly if you experience any of the symptoms described above. Early diagnosis and treatment can help prevent disease progression and reduce the risk of serious complications.
Causes of Hemangiopericytoma
The exact cause of hemangiopericytoma is still unknown. However, research has suggested several possible contributing factors:
- Genetic alterations: Changes or mutations in specific genes may play a role in the development of soft tissue sarcomas, including hemangiopericytoma.
- Association with other cancers: Limited studies have indicated a possible relationship between soft tissue sarcomas and the development of other types of cancer.
Risk Factors for Hemangiopericytoma
Hemangiopericytoma can develop in anyone, but certain groups appear to be at higher risk:
- Adults: The condition is far more common in adults than in children.
- Genetic predisposition: Individuals with a family history of sarcomas or related inherited disorders may have a higher likelihood of developing hemangiopericytoma.
- Toxic chemical exposure: Long-term exposure to harmful substances such as herbicides or vinyl chloride may increase the risk of this tumor.

Factors That Increase the Risk of Hemangiopericytoma
Non-modifiable factors
Genetics: Inherited mutations or a family history of related conditions may increase susceptibility to tumor formation.
Environmental exposure: Contact with certain toxic chemicals has been linked to a higher risk, including:
- Herbicides: Commonly used in agriculture to control weeds.
- Vinyl chloride: A chemical used in plastics manufacturing.
Modifiable factors
At present, there are no clearly defined risk factors that can be directly controlled to prevent hemangiopericytoma. However, general preventive measures can help maintain overall health and may support early detection:
- Healthy diet: Emphasize fruits, vegetables, and fiber-rich foods.
- Regular exercise: Helps maintain a healthy weight and cardiovascular fitness.
- Routine health checkups: Allow for early detection of abnormalities.
Diagnosis and Testing for Hemangiopericytoma
Your doctor will begin with a thorough physical examination, evaluation of clinical symptoms, and a review of your personal and family medical history.
To determine the tumor’s location, size, and degree of invasion, several imaging tests are commonly ordered:
- X-ray: Provides an initial view of abnormal masses or changes in bone and soft tissue.
- Magnetic Resonance Imaging (MRI): Produces detailed images of soft tissues, allowing precise assessment of tumor structure and infiltration into adjacent areas.
- Computed Tomography (CT) Scan: Creates detailed 3D cross-sectional images to help define the tumor’s size and exact location.
- Bone Scans: Detects whether the tumor has spread to the bones (used when metastasis is suspected)

In addition to imaging, your doctor may perform a biopsy. This is the definitive diagnostic procedure. A small tissue sample is taken from the tumor—usually through a minimally invasive technique—and examined under a microscope. Biopsy results help determine:
- The nature of the tumor: Whether it is benign or malignant
- Differentiation from other cancer types: Based on the cellular appearance
If the tumor is confirmed malignant, your doctor will proceed with staging to assess how far it has spread:
- Localized tumor: Confined to its original site or immediately surrounding tissues.
- Metastatic tumor: Has spread to the lungs, bones, or other organs.
Treatment of Hemangiopericytoma
Management of hemangiopericytoma depends on the tumor’s location, size, benign or malignant nature, and whether it has metastasized. The main treatment options include:
Surgery
Surgery is the primary treatment, aiming to remove the tumor completely along with a margin of surrounding healthy tissue to reduce the risk of recurrence.
- Limb-sparing surgery: Used whenever possible to preserve the affected limb. The diseased bone, cartilage, or muscle is removed and reconstructed with bone grafts or prosthetic implants.
- Amputation: Considered when the tumor has invaded major nerves or blood vessels and limb preservation is not feasible.
- Minimally invasive endoscopic surgery: Particularly useful for skull-base tumors.
- Endoscopic Endonasal Approach (EEA): The surgeon accesses and removes the tumor through the nasal passages without external incisions, reducing cosmetic deformity and shortening recovery time.
Radiation Therapy
Radiation may be administered after surgery to destroy any remaining cancer cells or before surgery to shrink the tumor.
- Gamma Knife Radiosurgery: A highly focused form of radiation delivering precise beams to the tumor without open surgery. It is especially suitable for residual tumors after surgery or for late recurrences.

Chemotherapy
Chemotherapy is reserved for malignant or metastatic hemangiopericytomas. It works by inhibiting the growth and division of cancer cells but can also affect healthy cells, leading to side effects such as fatigue, nausea, hair loss, and increased susceptibility to infection.
Post-Treatment Care and Rehabilitation
- Rehabilitation therapy: Essential after limb-sparing surgery or amputation to help patients regain mobility and independence.
- Regular follow-up visits: Allow early detection of recurrence or metastasis and timely intervention.

Lifestyle and Prevention for Hemangiopericytoma
While there is no guaranteed way to prevent hemangiopericytoma, adopting healthy habits can support recovery, improve quality of life, and reduce the risk of recurrence.
Lifestyle Tips
- Light physical activity: Engage in gentle exercises such as yoga, walking, or swimming if recommended by your doctor. Participate in rehabilitation programs after surgery—especially important following amputation or limb-sparing procedures—to regain strength and mobility.
- Regular health monitoring: Attend follow-up appointments as scheduled to detect early signs of recurrence or metastasis.
- Postoperative wound care: Follow all instructions for cleaning and caring for the surgical site to prevent infection.
- Use assistive devices appropriately: Wear prosthetics or mobility aids as instructed by rehabilitation specialists.
- Emotional support: Consider psychological counseling or support groups to reduce stress and maintain a positive outlook.
Nutrition Tips
Increase nutrient-dense foods:
- Protein sources: Chicken, fish, eggs, soy products to promote wound healing and tissue repair.
- Vitamins and minerals: Leafy greens (spinach, broccoli) and fruits (oranges, apples) to strengthen the immune system.
- Antioxidants: Berries (blueberries, strawberries) and nuts (walnuts, almonds) may help reduce cancer recurrence risk.
Limit unhealthy foods: Cut back on processed foods, high-fat meals, and refined sugars.
Stay hydrated: Drink enough water daily to support normal body functions.
Small, frequent meals: Especially useful for patients undergoing chemotherapy to ease nausea and improve digestion.

Prevention of Hemangiopericytoma
There is currently no specific method to prevent hemangiopericytoma because its exact cause remains unclear. However, certain measures may help reduce overall risk and support general health:
- Maintain a healthy lifestyle: Eat a balanced diet, exercise regularly, and avoid excess weight or obesity.
- Limit exposure to harmful chemicals: Stay away from pesticides, vinyl chloride, and other industrial toxins whenever possible.
- Schedule regular health checkups: Routine screenings may help detect abnormalities at an early stage.
- Manage stress effectively: Adopt a positive mindset and relaxation techniques to support immune system function.
