Thymoma: Causes, Symptoms, and Treatment
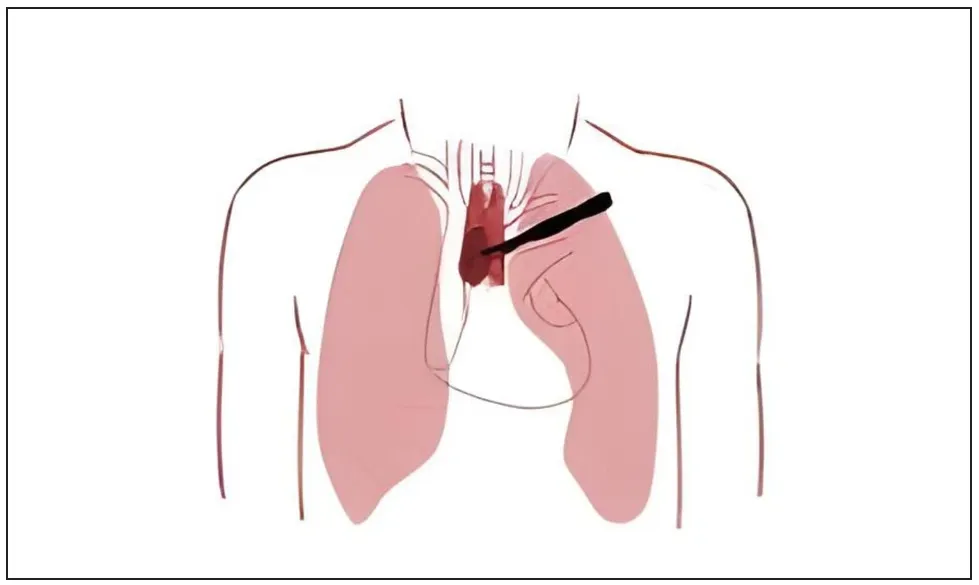
What is Thymoma?
Thymomas are often discovered incidentally on chest X-rays performed for other health reasons.
Key features of thymoma include:
- Cell characteristics: Cancer cells look similar to normal thymus cells, grow slowly, and rarely spread beyond the thymus.
- Association with autoimmune diseases: Thymoma is linked to autoimmune conditions such as myasthenia gravis, Good’s syndrome (hypogammaglobulinemia), and pure red cell aplasia.
Other, less common, related syndromes include polymyositis, lupus erythematosus, rheumatoid arthritis, thyroiditis, and Sjögren’s syndrome.
Thymoma differs from thymic carcinoma, which tends to be more aggressive. Distinguishing between these two is essential for proper treatment.
Symptoms of Thymoma
In the early stages, thymoma may not cause noticeable symptoms. As the tumor grows or causes paraneoplastic syndromes, symptoms may include:
- Chest pain or pressure
- Persistent cough without a clear cause
- Shortness of breath or a feeling of breathlessness
- Difficulty swallowing
When the tumor compresses the superior vena cava, it can lead to severe symptoms such as:
- Coughing, shortness of breath
- Fatigue, dizziness, headaches
- Swelling of the neck, face, arms, and hands
- Prominent veins in the upper body
Symptoms linked to associated syndromes:
- Myasthenia gravis: Double vision, drooping eyelids, fatigue, muscle weakness.
- Pure red cell aplasia: Fatigue, pale skin, mucosal pallor.
- Good’s syndrome: Diarrhea, swollen lymph nodes, frequent infections.

Complications
Compression of nearby organs: Large tumors may press on the lungs, heart, superior vena cava, esophagus, and nerves, causing shortness of breath, chest pain, or superior vena cava syndrome.
Paraneoplastic syndromes: Generalized muscle weakness, drooping eyelids, respiratory muscle weakness, severe anemia, or immunodeficiency with recurrent infections.
Metastasis or recurrence: Especially in thymic carcinoma, spread to the lungs, liver, or bones can occur, causing related symptoms.
When to See a Doctor
Seek medical care immediately if you experience:
- Unexplained shortness of breath or persistent cough
- Chest pain or pressure
- Neuromuscular signs (weakness, drooping eyelids, double vision, or difficulty breathing)
- Recurrent infections, unexplained fever
- Swelling of the neck, face, or arms with visible veins
- Unexplained fatigue or weakness

Causes
The exact cause of thymoma is unclear, but it is associated with systemic conditions. About 30–40% of patients show symptoms of myasthenia gravis; an additional 5% present with other systemic syndromes like pure red cell aplasia, dermatomyositis, systemic lupus erythematosus, Cushing’s syndrome, or SIADH.
Risk Factors
Age: Most common in adults aged 40–75; peak incidence at 40–50.
Ethnicity: In the U.S., people of Asian or Pacific Islander descent are diagnosed more frequently than other groups.
Autoimmune disease: Myasthenia gravis, Good’s syndrome, or pure red cell aplasia often coexist with thymoma.
Immune-related conditions: Chronic immunodeficiency or recurrent infections may increase risk.
Other factors: Autoimmune thyroiditis, exposure to toxic chemicals or pollutants (although not clearly proven), and rare immune-related genetic syndromes.

Diagnosis
To diagnose thymoma, doctors evaluate symptoms, personal and family medical history, and look for paraneoplastic signs. Tests may include:
- Chest X-ray: Detects abnormal masses.
- CT scan: Most common imaging for size, location, and invasiveness.
- MRI: Detailed structural imaging; distinguishes thymoma from other mediastinal masses.
- PET or PET/CT: Uses radioactive tracers to identify cancer cells and evaluate spread.
- Biopsy: The only way to confirm thymoma or thymic carcinoma. May involve surgical excision, needle biopsy, or minimally invasive surgery.
- Blood tests: Check for immunoglobulin deficiency or anemia.
- Immune function tests: Detect autoimmune disorders like myasthenia gravis.

Treatment
Treatment depends on the stage, cancer type, and patient condition:
Surgery: Standard treatment for early-stage thymoma; removes the tumor and possibly nearby organs or lymph nodes. May be combined with radiation or chemotherapy postoperatively.
Radiation therapy: High-energy X-rays to kill or stop cancer cells from growing; used after surgery or as a primary treatment for unresectable or recurrent tumors.

Chemotherapy: Drugs to kill or slow cancer cells; can be given before surgery to shrink the tumor or for advanced stages.
Targeted therapy:
- TKIs (sunitinib, lenvatinib): Block growth signals.
- mTOR inhibitors (everolimus): Block proteins that promote cancer growth and blood vessel formation.
Immunotherapy: Stimulates the immune system to attack cancer cells (e.g., pembrolizumab for PD-1/PD-L1 inhibition).
Hormone therapy: Octreotide (sometimes with prednisone) for tumors with hormone receptors.
Lifestyle & Prevention
Follow-up care: Regular checkups to monitor tumor progression or complications.
Symptom management: Deep breathing exercises to improve lung capacity, adequate rest, avoid chest strain.
Gentle exercise: Yoga or walking to enhance overall health; avoid heavy exertion.
Stress reduction: Meditation or relaxation techniques to support immunity.
Avoid harmful exposures: No smoking; minimize exposure to toxic chemicals.

Dietary tips:
Recommended: Lean protein, fish, eggs, tofu, antioxidant-rich vegetables (broccoli, carrots, spinach, berries), omega-3 fats (salmon, mackerel, olive oil), whole grains, vitamin C and zinc-rich foods (oranges, kiwis, almonds, pumpkin seeds).
Limit: Alcohol, caffeine, sugary drinks, red meat, fried foods, refined sugar.
Hydration: 1.5–2 liters of water daily.
Prevention:
- Avoid chemical and toxin exposure.
- Strengthen the immune system with balanced diet, regular sleep, and exercise.
- Manage underlying autoimmune conditions.
- High-risk individuals (family history or aged 40–75) should have regular health checkups.
- Reduce chronic stress to protect immune health.
