Comprehensive Guide to Thalidomide: Uses, Dosage, Side Effects, and More
1. What is Thalidomide?
2. Overview of Thalidomide
Generic Name
Thalidomide
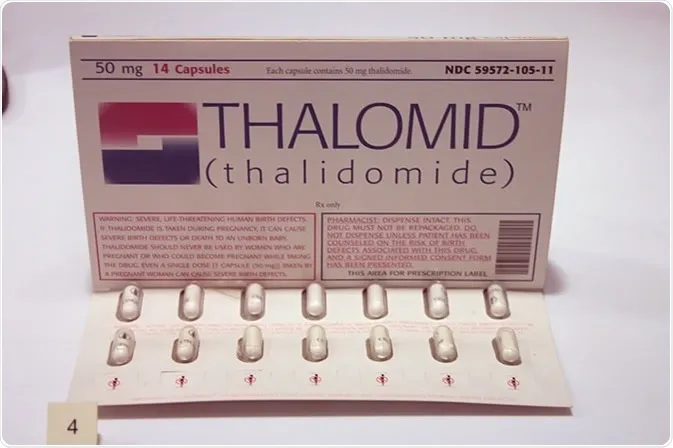
Brand Name
Thalomid, generics
Drug Group
Immunomodulatory agent (antineoplastic, anti-inflammatory)
Commonly Used For
This medication is used to:
- Treat multiple myeloma.
- Manage erythema nodosum leprosum (ENL).
- Control certain autoimmune conditions.
Key Characteristics
- Form: Oral capsules (50 mg, 100 mg, 150 mg, 200 mg) (detailed in Dosage section).
- Mechanism: Inhibits tumor necrosis factor-alpha (TNF-α), angiogenesis, and immune responses.
- Approval: FDA-approved (1998 for Thalomid) and EMA-approved for specific indications.
3. Indications and Uses of Thalidomide
Thalidomide is indicated for neoplastic, infectious, and autoimmune conditions, leveraging its multifaceted pharmacological effects:
- Multiple Myeloma: Treats newly diagnosed or relapsed multiple myeloma, often combined with dexamethasone or bortezomib, improving progression-free survival, per oncology guidelines.
- Erythema Nodosum Leprosum (ENL): Manages acute ENL in leprosy patients, reducing skin lesions and inflammation, supported by dermatology and infectious disease protocols.
- Myelodysplastic Syndromes (MDS): Used off-label to treat anemia in low-risk MDS, enhancing erythropoiesis, with evidence from hematology research.
- Crohn’s Disease: Investigated off-label for refractory Crohn’s disease, reducing inflammation and fistulae, supported by gastroenterology studies.
- Behçet’s Disease: Employed off-label to control oral ulcers and uveitis in Behçet’s disease, improving ocular outcomes, with rheumatology data.
- Aphthous Ulcers: Explored off-label for severe recurrent aphthous ulcers in HIV patients, reducing frequency, noted in infectious disease cohorts.
- Systemic Lupus Erythematosus (SLE): Used off-label to manage lupus nephritis, improving renal function, with emerging rheumatologic evidence.
- Kaposi’s Sarcoma: Investigated off-label for HIV-associated Kaposi’s sarcoma, reducing lesion growth, supported by oncology and infectious disease research.
- Glioblastoma Multiforme: Studied off-label as an adjunct in glioblastoma therapy, inhibiting angiogenesis, with preliminary neuro-oncology data.
Note: This drug requires strict monitoring due to teratogenicity; consult a healthcare provider for risk management and pregnancy prevention.
4. Dosage of Thalidomide
Important Note: The dosage of this immunomodulatory agent must be prescribed by a healthcare provider. Dosing varies by indication, patient response, and tolerance, with adjustments based on clinical evaluation.
Dosage for Adults
- Multiple Myeloma:
- Initial: 200 mg once daily at bedtime, often with dexamethasone (40 mg weekly).
- Maintenance: 50–200 mg daily, adjusted for response or toxicity, typically for 6–12 cycles.
- Erythema Nodosum Leprosum (ENL):
- Acute: 100–300 mg once daily, titrated to response (maximum 400 mg/day).
- Maintenance: 50–100 mg daily to prevent recurrence.
Dosage for Children
- ENL or Off-Label Use (12+ years):
- 1.5–2 mg/kg once daily, under pediatric specialist supervision.
- Not recommended under 12 years unless critical.
Dosage for Pregnant Women
- Pregnancy Category X: Contraindicated due to teratogenic risk; avoid unless life-saving. Use contraception and consult an obstetrician.
Dosage Adjustments
- Renal Impairment: No adjustment needed; monitor in severe cases (CrCl <30 mL/min).
- Hepatic Impairment: Reduce dose by 25–50% if severe (Child-Pugh C); monitor liver function.
- Elderly: Start with 100 mg once daily; increase cautiously to 200 mg if tolerated.
- Concomitant Medications: Adjust if combined with CYP1A2 inhibitors (e.g., ciprofloxacin), increasing levels.
Additional Considerations
- Take this active ingredient at bedtime with water, preferably after a light meal.
- Use with antiemetics if nausea occurs.
5. How to Use Thalidomide
- Administration:
- Swallow capsules whole with water, preferably at bedtime; avoid crushing or opening due to dust exposure risk.
- Take with a light meal to reduce gastrointestinal irritation.
- Timing: Use once daily at bedtime, maintaining consistency.
- Monitoring: Watch for drowsiness, rash, or signs of neuropathy (e.g., tingling).
- Additional Tips:
- Store at 15–30°C (59–86°F), protecting from moisture and light.
- Keep out of reach of children due to teratogenic risk.
- Report severe dizziness, numbness, or signs of allergic reaction immediately.
6. Contraindications for Thalidomide
This drug is contraindicated in:
- Pregnancy: Due to severe teratogenic effects (e.g., phocomelia).
- Hypersensitivity: Patients with a known allergy to Thalidomide or its components.
- Severe Neuropathy: Contraindicated due to worsening risk.
7. Warnings & Precautions for Thalidomide
General Warnings
- Teratogenicity: High risk of birth defects; mandatory contraception and pregnancy testing required.
- Peripheral Neuropathy: Risk of sensory or motor neuropathy; monitor regularly.
- Venous Thromboembolism: Increased risk of deep vein thrombosis (DVT) or pulmonary embolism; use prophylaxis.
- Drowsiness/Sedation: May impair alertness; avoid driving if affected.
- Bone Marrow Suppression: Risk of neutropenia or thrombocytopenia; monitor blood counts.
Additional Warnings
- Hepatotoxicity: Rare liver injury; check liver enzymes periodically.
- Hypersensitivity Reactions: Rare Stevens-Johnson syndrome; discontinue if rash worsens.
- Cardiotoxicity: Rare bradycardia or heart block; monitor ECG in at-risk patients.
- Seizures: Risk in patients with history; use cautiously.
- Infections: Increased susceptibility; monitor for signs.
Use in Specific Populations
- Pregnancy: Category X; contraindicated; use two forms of contraception.
- Breastfeeding: Avoid due to potential toxicity; monitor infant.
- Elderly: Higher risk of neuropathy; start with lower doses.
- Children: Limited to 12+ years; supervise closely.
- Renal/Hepatic Impairment: Adjust dose; avoid in severe cases.
Additional Precautions
- Inform your doctor about neuropathy, pregnancy plans, or medication history before starting this medication.
- Enroll in a risk evaluation and mitigation strategy (REMS) program if required.
8. Overdose and Management of Thalidomide
Overdose Symptoms
Overdose may cause:
- Drowsiness, confusion, or severe sedation.
- Severe cases: Coma, respiratory depression, or neuropathy exacerbation.
- Nausea, rash, or fatigue as early signs.
- Cardiovascular collapse with extremely high doses.
Immediate Actions
- Contact the Medical Team: Seek immediate medical help.
- Supportive Care: Administer activated charcoal if ingested recently, monitor vital signs, and provide IV fluids.
- Specific Treatment: Manage sedation with supportive care; no specific antidote.
- Monitor: Check neurological status, liver function, and heart rate for 24–48 hours.
Additional Notes
- Overdose risk is moderate; store securely.
- Report persistent symptoms (e.g., severe drowsiness, numbness) promptly.
9. Side Effects of Thalidomide
Common Side Effects
- Drowsiness (30–50%, managed with dose timing)
- Peripheral Neuropathy (20–40%, monitor for progression)
- Constipation (15–30%, relieved with fiber)
- Rash (10–25%, monitor for severity)
- Fatigue (10–20%, decreases with rest)
These effects may subside with dose adjustment or supportive care.
Serious Side Effects
Seek immediate medical attention for:
- Teratogenic: Birth defects if used during pregnancy.
- Neurological: Severe neuropathy or seizures.
- Cardiovascular: DVT, pulmonary embolism, or bradycardia.
- Hepatic: Jaundice or liver failure.
- Allergic: Rash, angioedema, or Stevens-Johnson syndrome.
Additional Notes
- Regular monitoring for neuropathy, blood counts, and liver function is advised.
- Report any unusual symptoms (e.g., leg swelling, severe weakness) immediately to a healthcare provider.
10. Drug Interactions with Thalidomide
This active ingredient may interact with:
- Sedatives: Enhances drowsiness (e.g., benzodiazepines); avoid combinations.
- Anticoagulants: Increases bleeding risk (e.g., warfarin); monitor INR.
- CYP1A2 Inhibitors: Increases levels (e.g., fluvoxamine); adjust dose.
- Immunosuppressants: Potentiates effects (e.g., cyclosporine); monitor.
- Alcohol: Worsens sedation; avoid use.
Action: Provide your healthcare provider with a complete list of medications.
11. Patient Education or Lifestyle
- Medication Adherence: Take this immunomodulatory agent as prescribed, following the exact schedule, preferably at bedtime.
- Monitoring: Report numbness, rash, or leg swelling immediately.
- Lifestyle: Avoid alcohol; use compression stockings if at risk for DVT.
- Diet: Take with a light meal; increase fiber to prevent constipation.
- Emergency Awareness: Know signs of thromboembolism or neuropathy; seek care if present.
- Follow-Up: Schedule regular check-ups every 1–3 months to monitor neuropathy, blood counts, and pregnancy status.
12. Pharmacokinetics of Thalidomide
- Absorption: Well-absorbed orally (peak at 2–5 hours); enhanced with food.
- Distribution: Volume of distribution ~120 L; 55–66% protein-bound.
- Metabolism: Hepatic via non-enzymatic hydrolysis to multiple metabolites; minimal CYP involvement.
- Excretion: Primarily renal (0.7%) and fecal as unchanged drug; half-life 5–7 hours.
- Half-Life: 5–7 hours, with prolonged immunomodulatory effects.
13. Pharmacodynamics of Thalidomide
This drug exerts its effects by:
- Inhibiting TNF-α production, reducing inflammation in ENL and myeloma.
- Blocking angiogenesis, limiting tumor growth in multiple myeloma.
- Modulating T-cell responses, enhancing immune regulation.
- Exhibiting dose-dependent risks of neuropathy and sedation.
14. Storage of Thalidomide
- Temperature: Store at 15–30°C (59–86°F); protect from light.
- Protection: Keep in original container, away from moisture.
- Safety: Store in a locked container out of reach of children due to teratogenic risk.
- Disposal: Dispose of unused capsules per hazardous drug regulations or consult a pharmacist.
15. Frequently Asked Questions (FAQs)
Q: What does Thalidomide treat?
A: This medication treats multiple myeloma and ENL.
Q: Can this active ingredient cause neuropathy?
A: Yes, neuropathy may occur; report tingling or numbness.
Q: Is Thalidomide safe for children?
A: Yes, for 12+ years with a doctor’s guidance.
Q: How is this drug taken?
A: Orally as capsules once daily at bedtime, as directed.
Q: How long is Thalidomide treatment?
A: Varies by condition, often long-term with monitoring.
Q: Can I use Thalidomide if pregnant?
A: No, it’s contraindicated; consult a doctor.
16. Regulatory Information
This medication is approved by:
- U.S. Food and Drug Administration (FDA): Approved in 1998 (Thalomid) for multiple myeloma and ENL, with REMS program.
- European Medicines Agency (EMA): Approved for specific indications with strict controls.
- Other Agencies: Approved globally with pregnancy prevention programs; consult local guidelines.
17. References
- U.S. Food and Drug Administration (FDA). (2023). Thalomid (Thalidomide) Prescribing Information.
- Official FDA documentation detailing the drug’s approved uses, dosage, and safety.
- European Medicines Agency (EMA). (2023). Thalidomide Summary of Product Characteristics.
- EMA’s comprehensive information on the medication’s indications and precautions in Europe.
- National Institutes of Health (NIH). (2023). Thalidomide: MedlinePlus Drug Information.
- NIH resource providing detailed information on the drug’s uses, side effects, and precautions.
- World Health Organization (WHO). (2023). WHO Model List of Essential Medicines: Thalidomide.
- WHO’s inclusion of Thalidomide for leprosy and myeloma.
- Blood. (2022). Thalidomide in Multiple Myeloma Therapy.
- Peer-reviewed article on Thalidomide efficacy (note: access may require a subscription).
