Comprehensive Guide to Plerixafor: Uses, Dosage, Side Effects, and More
What is Plerixafor?
Overview of Plerixafor
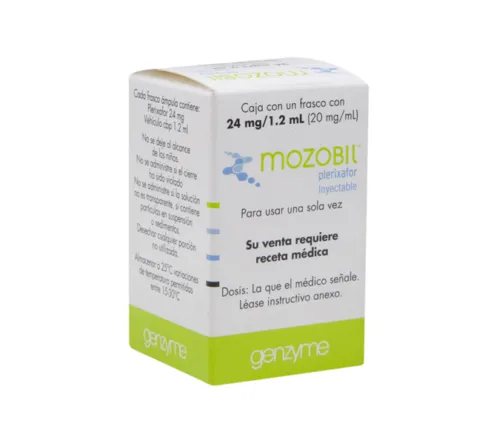
Generic Name: Plerixafor
Brand Name: Mozobil, generics
Drug Group: CXCR4 antagonist (hematopoietic stem cell mobilizer)
Commonly Used For
- Mobilize stem cells for autologous transplantation.
- Support treatment of hematologic malignancies.
- Enhance peripheral blood stem cell (PBSC) collection.
Key Characteristics
Form: Solution for subcutaneous injection (20 mg/mL, 1.2 mL or 2.4 mL vials) (detailed in Dosage section).
Mechanism: Blocks CXCR4/SDF-1 interaction, releasing CD34+ stem cells into circulation.
Approval: FDA-approved (2008 for Mozobil) and EMA-approved for stem cell mobilization.
Indications and Uses of Plerixafor
Plerixafor is indicated for stem cell mobilization and related therapeutic applications, leveraging its ability to enhance hematopoietic recovery:
Autologous Stem Cell Transplantation (Non-Hodgkin Lymphoma): Mobilizes CD34+ cells in patients with non-Hodgkin lymphoma (NHL) failing prior mobilization, improving transplant success, per ASH and EBMT guidelines.
Autologous Stem Cell Transplantation (Multiple Myeloma): Enhances stem cell yield in multiple myeloma patients for autologous transplant, reducing collection failures, supported by hematology trials.
Poor Mobilizers: Treats patients with inadequate stem cell mobilization after G-CSF alone, increasing CD34+ cell counts, with data from transplant studies.
Allogeneic Stem Cell Transplantation: Investigated off-label to mobilize donor stem cells in allogeneic settings, improving graft quality, with emerging transplant research.
Acute Myeloid Leukemia (AML) Remission: Explored off-label to mobilize leukemic stem cells for purging prior to transplant, enhancing remission rates, supported by oncology studies.
Aplastic Anemia: Used off-label to stimulate stem cell release in severe aplastic anemia, aiding recovery, with hematology evidence.
Sickle Cell Disease: Investigated off-label for stem cell mobilization in gene therapy or transplant for sickle cell disease, with preliminary data from genetic medicine.
Myelodysplastic Syndromes (MDS): Explored off-label to mobilize stem cells in MDS patients for transplant, improving outcomes, noted in hematologic research.
Solid Tumor Support: Studied off-label to enhance stem cell collection in patients with solid tumors (e.g., germ cell tumors) prior to high-dose chemotherapy, with supportive oncology data.
Immune Reconstitution: Investigated off-label to boost immune recovery post-transplant by mobilizing immune progenitor cells, with emerging immunology insights.
Dosage of Plerixafor
Dosage for Adults
Autologous Stem Cell Mobilization (with G-CSF): 0.24 mg/kg subcutaneous injection once daily for up to 4 consecutive days, administered 6–11 hours prior to apheresis, with G-CSF (e.g., 10 mcg/kg daily).
Multiple Myeloma or NHL: Same as above, with dose capped at 40 mg/day regardless of weight.
Dosage for Children
Autologous Stem Cell Mobilization (2–18 years, with G-CSF): 0.24 mg/kg subcutaneous injection once daily, adjusted for body surface area if needed, under pediatric hematologist supervision.
Not recommended under 2 years.
Dosage for Pregnant Women
Pregnancy Category D: Avoid unless benefits outweigh risks (e.g., life-saving transplant). Consult an obstetrician, with fetal monitoring.
Dosage Adjustments
Renal Impairment: Mild (CrCl 50–80 mL/min): No adjustment; moderate (CrCl 30–50 mL/min): Reduce to 0.16 mg/kg; severe (CrCl <30 mL/min): Avoid.
Hepatic Impairment: No specific adjustment; monitor in severe cases.
Elderly: Start with 0.16 mg/kg; increase to 0.24 mg/kg if tolerated.
Concomitant Medications: Adjust if combined with myelosuppressive agents, monitoring white blood cell counts.
Additional Considerations
- Administer this active ingredient subcutaneously in the abdominal area, rotating injection sites.
- Ensure G-CSF is given for 4 days prior to initiating this medication.
How to Use Plerixafor
Administration:
Inject subcutaneously into the abdominal area, avoiding the navel and scarred areas, using a prefilled syringe; rotate sites daily.
Administer 6–11 hours before apheresis, following G-CSF dosing.
Timing: Use once daily for up to 4 days, synchronized with collection schedule.
Monitoring: Watch for injection site reactions, abdominal pain, or signs of leukocytosis (e.g., fever).
Additional Tips:
- Store at 20–25°C (68–77°F) or refrigerate at 2–8°C (36–46°F); protect from light.
- Keep out of reach of children due to overdose risk.
- Report severe abdominal pain, shortness of breath, or signs of allergic reaction immediately.
Contraindications for Plerixafor
Hypersensitivity: Patients with a known allergy to Plerixafor or its components.
Severe Renal Impairment: Contraindicated if CrCl <30 mL/min due to accumulation risk.
Leukemia: Avoid in active leukemia due to leukocytosis risk.
Pregnancy: Contraindicated unless life-saving.
Side Effects of Plerixafor
Common Side Effects
- Injection Site Reactions (30–40%, manageable with rotation)
- Nausea (25–35%, relieved with antiemetics)
- Diarrhea (15–25%, transient)
- Fatigue (10–20%, decreases with rest)
- Headache (5–15%, relieved with hydration)
These effects may subside with dose adjustment or supportive care.
Serious Side Effects
Seek immediate medical attention for:
- Splenic: Rupture or enlargement.
- Hematologic: Severe leukocytosis or thrombocytopenia.
- Cardiovascular: Hypotension or tachycardia.
- Respiratory: Dyspnea or hypoxia.
- Allergic: Rash, angioedema, or anaphylaxis.
Additional Notes
- Regular monitoring for CBC, spleen size, and injection sites is advised.
- Report any unusual symptoms (e.g., severe abdominal pain, fever) immediately to a healthcare provider.
Warnings & Precautions for Plerixafor
General Warnings
Splenic Rupture: Rare but serious risk; monitor for left upper quadrant pain.
Leukocytosis: Risk of excessive white blood cell counts; monitor CBC daily.
Thrombocytopenia: Potential drop in platelets; assess bleeding risk.
Injection Site Reactions: Common redness or swelling; rotate sites.
Tumor Cell Mobilization: Risk of mobilizing malignant cells; screen patients.
Additional Warnings
Hypersensitivity Reactions: Rare anaphylaxis; discontinue if swelling occurs.
Cardiovascular Events: Rare hypotension or tachycardia; monitor vitals.
Gastrointestinal Distress: Nausea or diarrhea; use antiemetics if needed.
Bone Pain: Common with G-CSF combination; manage with analgesics.
Fetal Toxicity: Potential harm; use contraception during therapy.
Use in Specific Populations
- Pregnancy: Category D; avoid unless critical; use contraception.
- Breastfeeding: Avoid due to potential toxicity; monitor infant.
- Elderly: Higher risk of side effects; start with lower doses.
- Children: Limited to 2+ years; supervise closely.
- Renal/Hepatic Impairment: Adjust dose; avoid in severe cases.
Additional Precautions
- Inform your doctor about kidney disease, recent infections, or prior transplant history before starting this medication.
- Avoid abrupt cessation; complete the mobilization cycle as planned.
Overdose and Management of Plerixafor
Overdose Symptoms
- Leukocytosis, abdominal pain, or injection site reactions.
- Severe cases: Splenic rupture, hypotension, or respiratory distress.
- Nausea, dizziness, or fatigue as early signs.
- Seizures with extremely high doses.
Immediate Actions
Contact the Medical Team: Seek immediate medical help.
Supportive Care: Administer IV fluids, monitor vital signs, and manage leukocytosis with leukapheresis if needed.
Specific Treatment: No antidote; manage symptoms and monitor spleen size via ultrasound.
Monitor: Check CBC, liver function, and vital signs for 24–72 hours.
Additional Notes
- Overdose risk is low; store securely.
- Report persistent symptoms (e.g., severe pain, shortness of breath) promptly.
Drug Interactions with Plerixafor
This active ingredient may interact with:
- G-CSF: Enhances mobilization; monitor for excessive leukocytosis.
- Myelosuppressive Agents: Increases toxicity (e.g., chemotherapy); adjust timing.
- Anticoagulants: Alters bleeding risk; monitor INR.
- CYP450 Inhibitors/Inducers: Minimal effect; monitor if combined.
- Immunosuppressants: May affect stem cell yield; consult specialist.
Action: Provide your healthcare provider with a complete list of medications.
Patient Education or Lifestyle
Medication Adherence: Take this CXCR4 antagonist as prescribed in the mobilization schedule, following the exact timing.
Monitoring: Report abdominal pain, fever, or injection site issues immediately.
Lifestyle: Stay hydrated; avoid strenuous activity during mobilization.
Diet: Take with or without food; avoid heavy meals if nauseated.
Emergency Awareness: Know signs of splenic rupture or allergic reaction; seek care if present.
Follow-Up: Schedule regular check-ups daily during mobilization to monitor CBC, spleen size, and stem cell yield.
Pharmacokinetics of Plerixafor
Absorption: Well-absorbed subcutaneously (peak at 0.5–1 hour); unaffected by food.
Distribution: Volume of distribution ~0.3 L/kg; 58% protein-bound.
Metabolism: Minimal hepatic metabolism; excreted largely unchanged.
Excretion: Primarily renal (70%) as unchanged drug; half-life 3–5 hours.
Half-Life: 3–5 hours, with rapid mobilization effect.
Pharmacodynamics of Plerixafor
This drug exerts its effects by:
Antagonizing CXCR4, disrupting SDF-1 binding, and releasing CD34+ stem cells.
Enhancing peripheral blood stem cell collection for transplantation.
Demonstrating dose-dependent leukocytosis and spleen enlargement risks.
Exhibiting synergistic effects with G-CSF for optimal mobilization.
Storage of Plerixafor
Temperature: Store at 20–25°C (68–77°F) or refrigerate at 2–8°C (36–46°F); protect from light.
Protection: Keep in original carton, away from heat.
Safety: Store in a locked container out of reach of children due to toxicity risk.
Disposal: Dispose of unused vials per hazardous drug regulations or consult a pharmacist.
Frequently Asked Questions (FAQs)
Q: What does Plerixafor treat?
A: This medication mobilizes stem cells for transplantation.
Q: Can this active ingredient cause abdominal pain?
A: Yes, abdominal pain may occur; report if severe.
Q: Is Plerixafor safe for children?
A: Yes, for 2+ years with a doctor’s guidance.
Q: How is this drug taken?
A: Via subcutaneous injection, as directed by a healthcare provider.
Q: How long is Plerixafor treatment?
A: Up to 4 days for mobilization.
Q: Can I use Plerixafor if pregnant?
A: No, avoid unless life-saving; consult a doctor.
Regulatory Information
This medication is approved by:
U.S. Food and Drug Administration (FDA): Approved in 2008 (Mozobil) for stem cell mobilization in NHL and multiple myeloma.
European Medicines Agency (EMA): Approved for autologous stem cell mobilization.
Other Agencies: Approved globally for transplant support; consult local guidelines.
References
- U.S. Food and Drug Administration (FDA). (2023). Mozobil (Plerixafor) Prescribing Information.
- Official FDA documentation detailing the drug’s approved uses, dosage, and safety.
- European Medicines Agency (EMA). (2023). Plerixafor Summary of Product Characteristics.
- EMA’s comprehensive information on the medication’s indications and precautions in Europe.
- National Institutes of Health (NIH). (2023). Plerixafor: MedlinePlus Drug Information.
- NIH resource providing detailed information on the drug’s uses, side effects, and precautions.
- World Health Organization (WHO). (2023). WHO Guidelines on Stem Cell Transplantation.
- WHO’s recommendations for stem cell mobilization therapies.
- Blood. (2022). Plerixafor in Stem Cell Mobilization.
- Peer-reviewed article on Plerixafor efficacy (note: access may require a subscription).
