Comprehensive Guide to Nadolol: Uses, Dosage, Side Effects, and More
What is Nadolol?
Overview of Nadolol
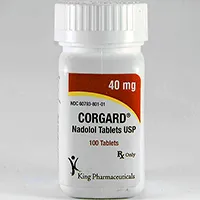
Generic Name: Nadolol
Brand Name: Corgard, generics
Drug Group: Beta-blocker (non-selective, antihypertensive, antianginal)
Commonly Used For
- Treat hypertension (high blood pressure).
- Manage angina pectoris.
- Prevent migraine headaches.
Key Characteristics
Form: Oral tablets (20 mg, 40 mg, 80 mg, 120 mg, 160 mg) (detailed in Dosage section).
Mechanism: Blocks catecholamine effects on beta receptors, lowering heart rate and myocardial oxygen demand.
Approval: FDA-approved (1978 for Corgard) and EMA-approved for hypertension and angina.
Indications and Uses of Nadolol
Nadolol is indicated for a variety of cardiovascular and neurological conditions, leveraging its non-selective beta-blocking properties:
Hypertension: Lowers blood pressure in essential hypertension, per cardiology guidelines, supported by clinical trials showing a 10–15 mmHg reduction in systolic pressure.
Angina Pectoris: Reduces chest pain frequency and severity in stable angina, improving exercise tolerance, recommended in cardiovascular protocols with evidence of reduced ischemic episodes.
Migraine Prophylaxis: Prevents migraine attacks, decreasing frequency by 50% in some patients, with neurology data.
Arrhythmias: Investigated off-label to control supraventricular tachycardia, with electrophysiology evidence.
Heart Failure (Adjunctive): Managed off-label in stable heart failure to reduce workload, with cardiology research.
Thyrotoxicosis: Used off-label to alleviate tachycardia and tremors, with endocrinology studies.
Portal Hypertension: Explored off-label in cirrhosis to prevent variceal bleeding, with hepatology data.
Anxiety-Related Tachycardia: Initiated off-label to manage situational heart rate increases, with psychiatry evidence.
Tremors (Essential): Applied off-label to reduce amplitude in essential tremor, with neurology research.
Post-Myocardial Infarction: Investigated off-label to improve survival rates, with cardiology studies.
Dosage of Nadolol
Dosage for Adults
Hypertension: Initial: 40 mg once daily, titrated to 80–320 mg daily based on response, taken with or without food.
Angina Pectoris: Initial: 40 mg once daily, increased to 80–240 mg daily, adjusted to control symptoms and maintain heart rate >50 bpm.
Migraine Prophylaxis: 40–80 mg once daily, with a maximum of 160 mg, tailored to reduce migraine frequency.
Dosage for Children (Off-Label)
Hypertension or Arrhythmias:
Initial: 0.5–1 mg/kg once daily, titrated under pediatric cardiology supervision, with a maximum of 2 mg/kg or 40 mg/day.
Dosage for Pregnant Women
Pregnancy Category C: Use only if benefits outweigh risks; consult an obstetrician and cardiologist, with fetal monitoring.
Dosage Adjustments
Renal Impairment:
- Mild (CrCl 31–60 mL/min): No adjustment; monitor closely.
- Moderate to Severe (CrCl <30 mL/min): Reduce dose by 50% and extend dosing interval to every 24–48 hours.
Hepatic Impairment: Mild to moderate (Child-Pugh A or B): Use cautiously; severe (Child-Pugh C): Avoid due to limited data.
Concomitant Medications: Adjust if combined with other antihypertensives (e.g., diuretics) or antiarrhythmics; monitor blood pressure.
Elderly: Start with 20 mg daily; titrate slowly to avoid bradycardia.
Abrupt Withdrawal: Taper over 1–2 weeks to prevent rebound hypertension or tachycardia.
Additional Considerations
- Take this active ingredient with water, with or without food, at a consistent time daily.
- Avoid crushing or chewing tablets; swallow whole to ensure sustained release.
How to Use Nadolol
Administration:
- Oral: Swallow tablets whole with a full glass of water, taken once daily, preferably in the morning.
- Take with or without food, but maintain a consistent pattern.
Timing: Administer at the same time daily to maintain steady blood levels.
Monitoring: Check pulse and blood pressure regularly; report rates <50 bpm or symptoms like dizziness immediately.
Additional Tips:
- Store at 20–25°C (68–77°F), protecting from moisture and light.
- Keep out of reach of children due to cardiac risk.
- Use a calendar or app to track doses and follow-up appointments.
- Educate patients on recognizing signs of overdose (e.g., extreme fatigue, fainting) and to avoid sudden cessation.
- Schedule baseline and follow-up ECGs every 1–3 months during dose adjustments to monitor heart function.
Contraindications for Nadolol
Hypersensitivity: Patients with a known allergy to Nadolol or other beta-blockers.
Severe Bradycardia: Contraindicated in heart rate <50 bpm or second-/third-degree AV block without a pacemaker.
Cardiogenic Shock: Avoid due to risk of worsening hemodynamic instability.
Uncompensated Heart Failure: Contraindicated until stabilized with other therapy.
Severe Asthma or COPD: Avoid due to bronchospasm risk from beta-2 blockade.
Pheochromocytoma: Contraindicated without alpha-blockade due to hypertensive crisis risk.
Severe Peripheral Arterial Disease: Avoid in critical limb ischemia due to reduced blood flow.
Side Effects of Nadolol
Common Side Effects
- Fatigue (10–20%, managed with rest)
- Dizziness (5–15%, reduced with hydration)
- Bradycardia (5–10%, monitored with pulse checks)
- Cold Extremities (3–8%, improves with warmth)
- Nausea (2–6%, relieved with food)
These effects may subside with adaptation.
Serious Side Effects
Seek immediate medical attention for:
- Cardiac: Heart block, heart failure, or asystole.
- Pulmonary: Bronchospasm or respiratory distress.
- Neurological: Syncope or seizures.
- Metabolic: Severe hypoglycemia in diabetics.
- Allergic: Rash, angioedema, or anaphylaxis (rare).
Additional Notes
Regular monitoring with ECG and blood pressure checks every 1–2 weeks is advised during dose titration.
Patients with diabetes should check glucose levels frequently due to masked hypoglycemia symptoms.
Report any unusual symptoms (e.g., chest pain, severe shortness of breath) immediately to a healthcare provider.
Long-term use (>6 months) requires periodic lung function tests in patients with respiratory history.
Warnings & Precautions for Nadolol
General Warnings
Bradycardia: Risk of excessive heart rate reduction; monitor pulse daily.
Heart Failure: Risk of decompensation; assess cardiac function before and during therapy.
Bronchospasm: Risk in patients with reactive airway disease; use with caution.
Hypotension: Risk of orthostatic hypotension; advise slow position changes.
Masking Hypoglycemia: Risk in diabetics; monitor blood glucose closely.
Additional Warnings
Abrupt Withdrawal: Risk of rebound tachycardia or myocardial infarction; taper over 1–2 weeks.
Peripheral Circulation: Risk of cold extremities or Raynaud’s phenomenon; monitor in at-risk patients.
Thyrotoxicosis: May mask symptoms; discontinue slowly if suspected.
Anesthesia: Risk of bradycardia during surgery; inform anesthesiologist.
Hypersensitivity Reactions: Rare rash or angioedema; stop if severe.
Use in Specific Populations
- Pregnancy: Category C; use with caution, monitoring fetal heart rate.
- Breastfeeding: Use caution; monitor infant for bradycardia.
- Elderly: Higher risk of hypotension and bradycardia; start low and titrate slowly.
- Children: Safe off-label with pediatric oversight.
- Renal/Hepatic Impairment: Adjust dose or avoid in severe cases.
Additional Precautions
- Inform your doctor about asthma, diabetes, or heart conditions before starting this medication.
- Avoid abrupt cessation; taper under medical supervision.
- Use caution with exercise to prevent excessive heart rate drop.
Overdose and Management of Nadolol
Overdose Symptoms
- Bradycardia, hypotension, or dizziness.
- Severe cases: Heart block, cardiac arrest, or bronchospasm.
- Fatigue, confusion, or syncope as early signs.
- Coma or respiratory depression with extremely high doses.
Immediate Actions
Contact the Medical Team: Seek immediate medical help.
Supportive Care: Monitor vital signs, provide IV fluids, and administer atropine for bradycardia if needed.
Specific Treatment: Use glucagon (5–10 mg IV) for beta-blocker overdose, followed by beta-agonists (e.g., isoproterenol) if unresponsive.
Monitor: Check ECG, blood pressure, and glucose for 24–48 hours.
Patient Education: Advise against doubling doses and to store safely.
Additional Notes
- Overdose risk is significant with accidental ingestion; store securely.
- Report persistent symptoms (e.g., severe dizziness, shortness of breath) promptly.
Drug Interactions with Nadolol
This active ingredient may interact with:
- Other Beta-Blockers: Increases bradycardia risk; avoid combination.
- Calcium Channel Blockers: Potentiates hypotension and AV block (e.g., verapamil); monitor.
- Insulin/Diuretics: Masks hypoglycemia; adjust diabetes management.
- Antiarrhythmics: Enhances conduction delays (e.g., amiodarone); use cautiously.
- NSAIDs: Reduces antihypertensive effect; monitor blood pressure.
Action: Provide your healthcare provider with a complete list of medications.
Patient Education or Lifestyle
Medication Adherence: Take this beta-blocker as prescribed for hypertension or angina, following the daily schedule.
Monitoring: Report bradycardia, dizziness, or signs of heart failure immediately.
Lifestyle: Avoid sudden exertion; limit alcohol to support blood pressure control.
Diet: Take with or without food; maintain a low-sodium diet.
Emergency Awareness: Know signs of overdose or withdrawal; seek care if present.
Follow-Up: Schedule regular check-ups every 1–3 months to monitor heart rate and blood pressure.
Pharmacokinetics of Nadolol
Absorption: Oral, peak at 2–4 hours; bioavailability ~30% due to first-pass metabolism.
Distribution: Volume of distribution ~1.5–2 L/kg; 30% protein-bound.
Metabolism: Minimal hepatic metabolism; excreted unchanged.
Excretion: Primarily renal (70–80% unchanged); half-life 10–24 hours.
Half-Life: 10–24 hours, prolonged in renal impairment.
Pharmacodynamics of Nadolol
This drug exerts its effects by:
Non-selectively blocking beta-1 and beta-2 receptors, reducing heart rate and contractility.
Lowering blood pressure and myocardial oxygen demand in hypertension and angina.
Exhibiting dose-dependent risks of bradycardia and bronchospasm.
Storage of Nadolol
- Temperature: Store at 20–25°C (68–77°F); protect from moisture and light.
- Protection: Keep in original container, away from heat and humidity.
- Safety: Store in a secure location out of reach of children and pets due to cardiac risk.
- Disposal: Dispose of unused tablets per local regulations or consult a pharmacist.
Frequently Asked Questions (FAQs)
Q: What does Nadolol treat?
A: This medication treats high blood pressure and angina.
Q: Can this active ingredient cause fatigue?
A: Yes, fatigue is common; report if severe.
Q: Is Nadolol safe for children?
A: Yes, off-label with supervision.
Q: How is this drug taken?
A: Orally as tablets, once daily.
Q: How long is Nadolol treatment?
A: Often long-term, with periodic review.
Q: Can I use Nadolol if pregnant?
A: Yes, with caution; consult a doctor.
Regulatory Information
This medication is approved by:
U.S. Food and Drug Administration (FDA): Approved in 1978 (Corgard) for hypertension and angina.
European Medicines Agency (EMA): Approved for cardiovascular conditions.
Other Agencies: Approved globally for beta-blockade; consult local guidelines.
References
- U.S. Food and Drug Administration (FDA). (2023). Corgard (Nadolol) Prescribing Information.
- Official FDA documentation detailing the drug’s approved uses, dosage, and safety.
- European Medicines Agency (EMA). (2023). Nadolol Summary of Product Characteristics.
- EMA’s comprehensive information on the medication’s indications and precautions in Europe.
- National Institutes of Health (NIH). (2023). Nadolol: MedlinePlus Drug Information.
- NIH resource providing detailed information on the drug’s uses, side effects, and precautions.
- World Health Organization (WHO). (2023). WHO Model List of Essential Medicines: Nadolol.
- WHO’s consideration of Nadolol for cardiovascular conditions.
- Journal of the American College of Cardiology. (2022). Nadolol in Hypertension.
- Peer-reviewed article on Nadolol efficacy (note: access may require a subscription).
