Comprehensive Guide to Lidocaine: Uses, Dosage, Side Effects, and More
What is Lidocaine?
Overview of Lidocaine
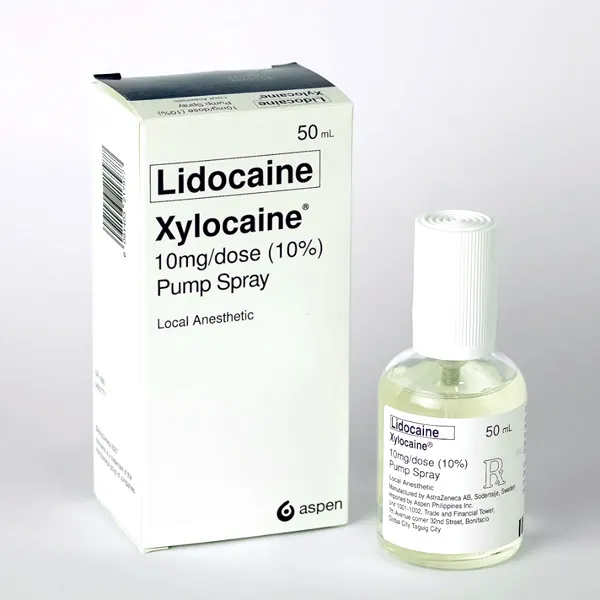
Generic Name: Lidocaine
Brand Name: Xylocaine, Lidoderm, generics
Drug Group: Local anesthetic, antiarrhythmic (Class IB)
Commonly Used For
- Provide local anesthesia during procedures.
- Relieve neuropathic pain.
- Treat ventricular arrhythmias.
Key Characteristics
Form: Injectable solutions (0.5%, 1%, 2%), topical patches (5%), creams, gels, or IV infusions (detailed in Dosage section).
Mechanism: Inhibits sodium influx, stabilizing neuronal and cardiac membranes.
Approval: FDA-approved (1948 for Xylocaine) and EMA-approved for anesthesia and arrhythmias.
Indications and Uses of Lidocaine
Lidocaine is indicated for a variety of anesthetic, analgesic, and cardiac conditions, leveraging its sodium channel-blocking properties:
Local Anesthesia: Provides numbness for dental procedures, minor surgeries, or skin biopsies, per anesthesiology guidelines, supported by clinical trials showing rapid onset within 1–2 minutes.
Neuropathic Pain: Manages post-herpetic neuralgia or diabetic neuropathy with topical patches, reducing pain scores by 30–50%, recommended in pain management protocols.
Ventricular Arrhythmias: Treats life-threatening ventricular tachycardia or fibrillation, improving survival rates, with cardiology evidence.
Epidural Anesthesia: Used for labor pain or cesarean sections, enhancing maternal comfort, per obstetric anesthesiology studies.
Regional Nerve Blocks: Applied for upper or lower limb surgeries, providing targeted analgesia, with orthopedic surgery data.
Burn Wound Care: Investigated off-label to reduce pain during dressing changes, with burn unit research.
Chronic Pain Syndromes: Explored off-label for fibromyalgia or complex regional pain syndrome, with rheumatology-pain medicine evidence.
Status Epilepticus: Managed off-label as an adjunct to control seizures, with neurology studies.
Oral Ulcers: Initiated off-label to alleviate pain from aphthous ulcers, with dental medicine data.
Postoperative Ileus: Used off-label to enhance gastrointestinal motility post-surgery, with surgical gastroenterology research.
Dosage of Lidocaine
Dosage for Adults
Local Infiltration (Anesthesia):
- 0.5% or 1% solution: 1–5 mL (5–50 mg) per site, up to 4.5 mg/kg (max 300 mg) without epinephrine, or 7 mg/kg (max 500 mg) with epinephrine.
Topical Pain Relief (Neuropathic Pain):
- 5% patch: Apply up to 3 patches for 12 hours on/off daily to affected area.
Ventricular Arrhythmias (IV):
- Loading dose: 1–1.5 mg/kg IV bolus over 2–3 minutes, followed by 1–4 mg/min infusion; max 300 mg over 1 hour.
Dosage for Children (≥1 year)
Local Anesthesia:
- 0.5%–1% solution: 3–5 mg/kg per site, up to 7 mg/kg with epinephrine, under pediatric anesthesiology supervision.
Arrhythmias (IV, Off-Label):
- Loading dose: 0.5–1 mg/kg, followed by 10–50 µg/kg/min infusion, with ECG monitoring.
Dosage for Pregnant Women
Pregnancy Category B: Use only if benefits outweigh risks; consult an obstetrician and anesthesiologist, with fetal monitoring.
Dosage Adjustments
Renal Impairment: Reduce infusion rate in severe cases (CrCl <30 mL/min); monitor plasma levels.
Hepatic Impairment: Mild to moderate (Child-Pugh A or B): Use cautiously; severe (Child-Pugh C): Avoid due to reduced clearance.
Concomitant Medications: Adjust if combined with beta-blockers or cimetidine, increasing toxicity risk; monitor levels.
Elderly: Start with lower doses (e.g., 1 mg/kg); monitor for CNS toxicity.
Max Dose: Limit total dose based on weight and epinephrine use to prevent systemic effects.
Additional Considerations
- Administer this active ingredient with epinephrine (1:200,000) to prolong effect and reduce systemic absorption, if appropriate.
- Use preservative-free formulations for spinal or epidural administration.
- Monitor plasma levels (therapeutic range 1.5–5 µg/mL) in prolonged IV use.
How to Use Lidocaine
Administration:
- Injection: Use a fine needle for infiltration or nerve block, aspirate to avoid intravascular injection.
- Topical: Apply patch or gel to intact skin, covering the painful area, and remove after 12 hours.
- IV: Administer bolus slowly under ECG monitoring, followed by continuous infusion.
Timing: Apply or inject as needed for procedures, with patches used in a 12-hour on/off cycle.
Monitoring: Watch for dizziness, tinnitus, or signs of toxicity (e.g., seizures); report changes immediately.
Additional Tips:
- Store at 15–30°C (59–86°F), protecting from light and freezing; discard opened vials after 24 hours.
- Keep out of reach of children; use gloves when applying topical forms to avoid absorption.
- Educate patients on patch removal and site rotation to prevent skin irritation.
- Schedule regular ECG and neurological assessments during IV therapy to detect arrhythmias or CNS effects.
- Avoid applying near eyes or mucous membranes unless directed by a provider.
Contraindications for Lidocaine
Hypersensitivity: Patients with a known allergy to Lidocaine or amide-type anesthetics.
Severe Heart Block: Contraindicated in second- or third-degree AV block without a pacemaker.
Adams-Stokes Syndrome: Avoid due to risk of asystole.
Severe Hypovolemia: Contraindicated due to reduced cardiac output.
Concurrent Use with Certain Drugs: Avoid with Class III antiarrhythmics (e.g., amiodarone) due to proarrhythmic risk.
Infected Tissue: Avoid injection into infected or inflamed areas to prevent systemic spread.
Myasthenia Gravis: Contraindicated due to potential muscle weakness exacerbation.
Side Effects of Lidocaine
Common Side Effects
- Dizziness (10–20%, temporary, resolves with rest)
- Numbness (5–15%, localized to application site)
- Injection Site Pain (5–10%, decreases with proper technique)
- Headache (3–8%, managed with hydration)
- Nausea (2–6%, relieved with antiemetics)
These effects may subside with adaptation or dose adjustment.
Serious Side Effects
Seek immediate medical attention for:
- Neurological: Seizures, coma, or respiratory depression.
- Cardiac: Bradycardia, ventricular fibrillation, or asystole.
- Metabolic: Methemoglobinemia or acidosis.
- Allergic: Anaphylaxis or angioedema.
- Local: Tissue necrosis from extravasation.
Additional Notes
Regular monitoring with ECG and neurological exams is essential during IV use to detect toxicity early.
Patients with G6PD deficiency should be monitored for methemoglobinemia, with methylene blue available.
Report any unusual symptoms (e.g., blue lips, irregular heartbeat) immediately to a healthcare provider.
Long-term topical use (>14 days) requires skin assessments to prevent irritation or sensitization.
Warnings & Precautions for Lidocaine
General Warnings
CNS Toxicity: Risk of seizures or coma with overdose; monitor for early signs like tinnitus or confusion.
Cardiac Toxicity: Risk of bradycardia or asystole with IV use; monitor ECG continuously.
Methemoglobinemia: Rare risk with topical or high-dose use; assess oxygen saturation.
Hypersensitivity Reactions: Risk of anaphylaxis; discontinue if rash or swelling occurs.
Malignant Hyperthermia: Rare trigger in susceptible patients; have dantrolene available.
Additional Warnings
Liver Dysfunction: Risk of accumulation; monitor liver enzymes in chronic use.
Respiratory Depression: Risk with high spinal doses; monitor breathing.
Drug Interactions: Risk of toxicity with CYP3A4 inhibitors (e.g., erythromycin); adjust dose.
Pregnancy Risks: Potential fetal bradycardia; use lowest effective dose.
Elderly Sensitivity: Higher risk of CNS effects; start with reduced doses.
Use in Specific Populations
- Pregnancy: Category B; use with caution, monitoring fetal heart rate.
- Breastfeeding: Use caution; monitor infant for sedation.
- Elderly: Higher toxicity risk; adjust dose and monitor closely.
- Children: Safe with pediatric oversight for anesthesia.
- Renal/Hepatic Impairment: Adjust or avoid in severe cases.
Additional Precautions
- Inform your doctor about liver disease, heart conditions, or drug allergies before starting this medication.
- Avoid self-administering topical forms near open wounds or burns.
- Use with ECG monitoring for IV administration to detect arrhythmias early.
Overdose and Management of Lidocaine
Overdose Symptoms
- Mild dizziness, tinnitus, or numbness.
- Severe cases: Seizures, respiratory arrest, or cardiac arrest.
- Slurred speech, muscle twitching, or hypotension as early signs.
- Coma or profound bradycardia with extremely high doses.
Immediate Actions
Contact the Medical Team: Seek immediate medical help if toxicity signs appear.
Supportive Care: Secure airway, provide oxygen, and support ventilation if needed.
Specific Treatment: Use benzodiazepines (e.g., diazepam) for seizures and lipid emulsion (e.g., Intralipid) for systemic toxicity.
Monitor: Check ECG, plasma levels (target <5 µg/mL), and neurological status for 24–48 hours.
Patient Education: Advise against exceeding prescribed doses and to report accidental ingestion immediately.
Additional Notes
- Overdose risk is linked to rapid IV administration or excessive topical use; store securely.
- Report persistent symptoms (e.g., chest pain, severe confusion) promptly to prevent complications.
Drug Interactions with Lidocaine
This active ingredient may interact with:
- Beta-Blockers: Increases toxicity (e.g., propranolol); monitor levels.
- Cimetidine: Reduces clearance; adjust dose.
- Class III Antiarrhythmics: Potentiates QT prolongation (e.g., sotalol); avoid.
- Neuromuscular Blockers: Enhances paralysis risk; use cautiously.
- Opioids: Amplifies sedation; monitor respiratory status.
Action: Provide your healthcare provider with a complete list of medications.
Patient Education or Lifestyle
Medication Adherence: Use this local anesthetic as prescribed for pain or arrhythmias, following the administration schedule.
Monitoring: Report dizziness, numbness, or signs of toxicity immediately.
Lifestyle: Avoid driving after topical or IV use until effects wear off.
Diet: No specific restrictions; maintain hydration.
Emergency Awareness: Know signs of overdose or allergic reaction; seek care if present.
Follow-Up: Schedule regular check-ups to monitor cardiac and neurological status during prolonged use.
Pharmacokinetics of Lidocaine
Absorption: Rapid via IV or mucosal routes; topical absorption varies (peak 1–2 hours).
Distribution: Volume of distribution ~1.1–1.3 L/kg; 60–80% protein-bound.
Metabolism: Hepatic via CYP3A4 and CYP1A2 to monoethylglycinexylidide (MEGX) and glycinexylidide (GX).
Excretion: Primarily renal (90% as metabolites); half-life 1.5–2 hours.
Half-Life: 1.5–2 hours, prolonged in hepatic impairment.
Pharmacodynamics of Lidocaine
This drug exerts its effects by:
Blocking sodium channels in nerve fibers, preventing depolarization and pain signal transmission.
Stabilizing cardiac membranes to suppress ventricular arrhythmias.
Exhibiting dose-dependent risks of CNS and cardiac toxicity.
Storage of Lidocaine
- Temperature: Store at 15–30°C (59–86°F); protect from light and freezing.
- Protection: Keep in original container, away from heat and humidity.
- Safety: Store in a secure location out of reach of children and pets due to toxicity risk.
- Disposal: Dispose of unused vials or patches per local regulations or consult a pharmacist.
Frequently Asked Questions (FAQs)
Q: What does Lidocaine treat?
A: This medication treats pain and arrhythmias.
Q: Can this active ingredient cause dizziness?
A: Yes, dizziness is common; report if severe.
Q: Is Lidocaine safe for children?
A: Yes, with supervision for anesthesia.
Q: How is this drug taken?
A: Via injection, topical application, or IV, as directed.
Q: How long is Lidocaine effective?
A: 1–2 hours for injection, up to 12 hours for patches.
Q: Can I use Lidocaine if pregnant?
A: Yes, with caution; consult a doctor.
Regulatory Information
This medication is approved by:
U.S. Food and Drug Administration (FDA): Approved in 1948 (Xylocaine) for anesthesia and arrhythmias.
European Medicines Agency (EMA): Approved for local anesthesia and cardiac use.
Other Agencies: Approved globally for anesthetic and antiarrhythmic therapy; consult local guidelines.
References
- U.S. Food and Drug Administration (FDA). (2023). Xylocaine (Lidocaine) Prescribing Information.
- Official FDA documentation detailing the drug’s approved uses, dosage, and safety.
- European Medicines Agency (EMA). (2023). Lidocaine Summary of Product Characteristics.
- EMA’s comprehensive information on the medication’s indications and precautions in Europe.
- National Institutes of Health (NIH). (2023). Lidocaine: MedlinePlus Drug Information.
- NIH resource providing detailed information on the drug’s uses, side effects, and precautions.
- World Health Organization (WHO). (2023). WHO Model List of Essential Medicines: Lidocaine.
- WHO’s inclusion of Lidocaine for anesthesia and emergencies.
- Anesthesiology. (2022). Lidocaine in Neuropathic Pain.
- Peer-reviewed article on Lidocaine efficacy (note: access may require a subscription).
